The fish report

This page includes excerpts from The Fish Report. Download the full report for more information.
Over the last decade or so, the reputation of fish oils has undergone a meteoric rise from the dreaded cod liver oil of years gone by to the highly esteemed omega-3 fish oil capsules of the new millennia. If you want to keep up with modern nutrition you must be omega-3 savvy!
The alternative view is that the only thing ‘clever‘ about fish oils is the huge marketing campaign that has got thousands of people running to the health food shops. Fish oils are promoted everywhere you look – well-known scientists recommend them for children, TV adverts hint at their brain-boosting benefits, food producers slip them into all manner of foods. Health food shops struggle to meet demand. So convincing is the marketing that many people believe that oily fish are the only source of the magical omega-3 fatty acids which keep our hearts healthy, children clever and ward off allergies and inflammatory conditions such as arthritis.
We’re told that oily fish benefit heart health because of the omega-3 fats they contain. However, the evidence is inconclusive. One long-term study showed that men with heart disease, advised to eat oily fish or fish oil supplements, had a higher risk of sudden death from heart failure than men not so advised. Another study found fish oil supplements increased life-threatening abnormal heart rhythms in patients with implanted defibrillators.
A review of studies on fish oils and heart health (which included over half a million heart disease patients), showed no clear benefit of omega-3 fats on heart health. One possible explanation the authors suggest for this is the harmful effects of toxins found in oily fish. Many people are unaware that all the world’s oceans and rivers are contaminated with toxic pollutants such as polychlorinated biphenyls (PCBs), dioxins and mercury. These toxins accumulate, especially in fatty fish, as you move up the food chain and may completely cancel out any beneficial effects the omega-3s offer. So you are better off getting your omega-3s from healthy plant-based sources such as flaxseed oil, hempseed oil and walnuts. These foods are not laced with toxic pollutants.
This is why the Government has issued warnings to young people, pregnant and breast-feeding women, and those who may become pregnant one day, to limit how much oily fish they eat. Some governments warn that pregnant and breastfeeding women and children under 16 should not eat larger, older fish such as shark, marlin or swordfish because of the high levels of mercury present. Others have voiced concerns about the levels of dioxins in herring, salmon and mackerel, but most people know little about these risks. These pollutants can harm children and adults as well as unborn babies and infants.
More recently the Government has extended its warnings on dioxins and PCBs to include some non-oily fish including: sea bream, turbot, halibut, dog fish or huss, and sea bass. However, it also continues to recommend we eat oily fish. The mixed messages have left people understandably confused.
Farmed fish are not the answer. In general they tend to contain less omega-3s than their wild counterparts and more toxins. In fact, the levels of toxins in farmed fish are a significant concern to many scientists. A comparison of farmed salmon and wild salmon found that the farmed fish had consistently higher levels of contaminants, including PCBs. Other studies show similar findings. This could mean considerable health risks for those who regularly eat farmed salmon.
Fish is not a popular food in the UK; people eat only a third of a portion of oily fish a week with seven out of ten people consuming none at all. Promoting oily fish as a public health policy is clearly not working. The worst consequence of this is that more helpful advice on how to get omega-3s from plant-based foods is just not being given.
The good news is you don’t have to eat neurotoxins and carcinogens to get your omega-3s; there are perfectly safe plant sources. Many studies show that omega-3s from plants can protect health without exposing us to these harmful toxins. So as part of a vegetarian or vegan diet, plant-based omega-3s provide better protection from heart disease and many other degenerative conditions. This benefits the environment as well; plant-based sources of omega-3s are sustainable, fish are not.
Safer, healthier and sustainable sources of omega-3s include flaxseeds (linseeds), rapeseeds, soya, walnuts and oils made from them. Some species of algae (and supplements made from them) can provide the longer chain omega-3s found in oily fish without exposing you to harmful pollutants. By avoiding fish you can protect your health and help stop the destruction of the oceans caused by over-fishing.
The research clearly shows that fish oils are not the wonder food the industry would have you believe. They don’t guarantee good heart health and turn all kids into geniuses. They are not the answer to arthritis and other inflammatory conditions (which vegetarians suffer much less from). We must stop looking for a ‘quick fix’ and focus on the bigger picture. improving our diets by cutting out the foods laden with animal fats, sugar, salt and cholesterol and eating more fruit, vegetables, pulses, wholegrains, nuts and seeds.
This fully-referenced scientific report examines the science behind the health claims and reveals the research the fish industry would rather ignore. It describes why omega-3 fatty acids are important and explains why plant-based oils are better for human health and the environment. It also describes what toxic substances are found in fish and reveals how harmful they can be. It explains why public health policies promoting oily fish are misplaced and undermine more effective and sustainable strategies. It will leave you in no doubt – fish is not a health food.
Why do we need fat?
Most people regard all dietary fat as ‘bad’ or unhealthy but the body actually needs a moderate amount of fat (or fatty acids) to function properly. Besides being an energy source, fatty acids play a crucial structural role in all cell membranes; they help hold our cells together. They also help our bodies transport, break down and excrete cholesterol. They are used to make important hormone-like compounds called eicosanoids which regulate many processes in the body including inflammation and blood clotting. Fatty acids help maintain healthy hair and skin, they protect vital organs and keep the body insulated. They are also needed to transport the fat-soluble vitamins A, D, E and K, from food into the body. In summary, without some fats in the diet, we cannot function.
The chemical structure of fat:
Figure 1 shows how fatty acids are made up of chains of carbon atoms (the carbon backbone) that have hydrogen atoms attached to them. They are referred to as saturated, monounsaturated or polyunsaturated depending on the number of hydrogen atoms attached to the carbon backbone.
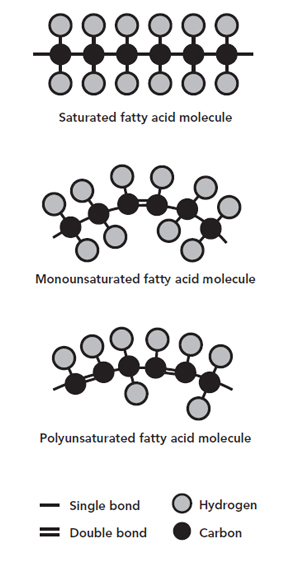
The links between the carbon atoms are called bonds and can be single or double. Saturated fatty acids have no double bonds and are fully ‘saturated’ with hydrogen atoms. Monounsaturated fats have one double bond and polyunsaturated fats have more than one. The way different fatty acids behave in the body is largely determined by the number and location of these double bonds.
Saturated fat:
As stated, saturated fats have the maximum number of hydrogen atoms attached to the carbon atoms. This makes the molecule less flexible. So these fats tend to be solid at room temperature, such as lard and butter.
Unsaturated fat:
Unsaturated (monounsaturated and polyunsaturated) fats tend to be liquid at room temperature, such as olive and sunflower oil. It is their flexible nature that makes these fats so biologically useful.
Cis and trans fats:
The usual shape of naturally occurring unsaturated fats is referred to as ‘cis’ (Latin for ‘on the same side’), as the hydrogen atoms face the same direction (see Figure 2). When the hydrogen atoms are oriented in opposing directions, the molecule is called a ‘trans’ fatty acid (trans means ‘across’ in Latin). Most trans fats are made industrially by adding hydrogen to unsaturated plant oils, in a process called hydrogenation. This process reshapes the double bonds, twisting them so that the hydrogen atoms end up on different sides of the chain.
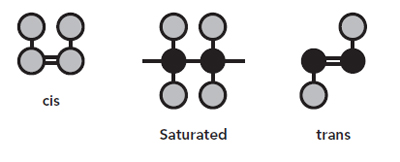
Figure 2: Cis and trans fatty acids configuration
While trans fats are made of exactly the same building blocks as non-trans fats, their different arrangement affects the physical properties of the fat. They are harder, have a higher melting point, and crucially, a longer shelf-life than their cis-shaped equivalents.
There is increasing evidence that trans fats are harmful to health. While both saturated and trans fats increase levels of LDL cholesterol (so-called ‘bad’ cholesterol), trans fats also lower levels of HDL cholesterol (‘good’ cholesterol), thus increasing the risk of heart disease. Indeed, some evidence suggests that trans fats may be even more harmful to health than saturated fats. This position is supported by a scientific review published in the New England Journal of Medicine in 2006 which states that the consumption of trans fatty acids results in considerable potential harm but no apparent benefit (Mozaffarian et al., 2006). Many health authorities worldwide agree and recommend that consumption of trans fat be reduced or avoided altogether.
God fat, bad fat:
We need a moderate amount of so-called ‘good’ fats in the diet. However, not all fats are created equal. As stated, some are beneficial, while others can be harmful. For example, as 60 per cent of the brain is made of fat, it is very important that it is provided with enough ‘bendy’ polyunsaturated fatty acids to stay supple and elastic in order to be able to respond to different stimuli such as hormones. If the cell membranes in the brain (and other parts of the body) are rigid they cannot react so well (Saldeen and Saldeen, 2006). This means that less flexible (more saturated) fats may take their place and normal functioning can be impaired.
Coldwater fish (salmon, mackerel, sardines and herring) need a high level of flexible polyunsaturated fats in their cell membranes to enable them to see and swim in cold, dark, watery environments. Just imagine replacing these flexible fats with those from a cold pat of butter (saturated fat), it would not work! Fish obtain their polyunsaturated fats from plankton, algae and other fish. These fats are also found in eggs and dairy foods (which also contain unhealthy saturated fats) and are plentiful in plant foods such as nuts and seeds and their oils, avocados and soya foods. Green leafy vegetables contain them too, but not much as they are a very low-fat food. Although olive oil contains some saturated fat, it is mainly made up of monounsaturated fat, which is a good substitute for butter, lard or omega-6 fats, such as sunflower oil, in cooking.
While unsaturated fats are an important part of our diets, we have absolutely no dietary requirement at all for saturated fat. Found widely in meat, dairy, eggs, poultry, processed foods and fish, this unhealthy type of fat contributes to the risk of heart disease and stroke by raising blood cholesterol levels.
Despite its reputation for containing unsaturated ‘healthy’ fats, much of the fat found in oily fish is saturated (see Table 1). For example, nearly 80 per cent of the calories in smoked mackerel come from fat and over half of the calories in grilled salmon come from fat. Around one-fifth of the total fat in both these types of fish is saturated (FSA, 2002).
Table 1: Nutritional content of selected oily fish and vegetarian alternatives
| 100 grams of: | Protein (grams) | Total fat (grams) | Saturated fat (grams) | Cholesterol (milligrams) | Fibre (grams) | Energy (kcals) |
|---|---|---|---|---|---|---|
| Grilled salmon | 24.2 | 13.1 | 2.5 | 60 | 0 | 215 |
| Smoked mackerel | 18.9 | 30.9 | 6.3 | 105 | 0 | 354 |
| Tinned sardines | 23.3 | 14.1 | 2.9 | 65 | 0 | 220 |
| Smoked tofu | 10.9 | 7.1 | 1.5 | 0 | 0.5 | 112 |
| Red lentils, boiled | 7.6 | 0.4 | Trace amounts | 0 | 1.9 | 100 |
| Kidney beans, boiled | 8.4 | 0.5 | 0.1 | 0 | 6.7 | 103 |
| Tinned chick peas | 10.3 | 2.5 | 0.2 | 0 | 4.3 | 119 |
| Vegetarian style fish fingers | 13.3 | 15.2 | 1.9 | 0 | 1.0 | 279 |
Fish and shellfish are also significant sources of cholesterol; some species containing nearly as much as steak. The amount of cholesterol in prawns is estimated to be around 280 milligrams per 100 grams; nearly four times as much as is found in a rump steak (FSA, 2002). Whichever way it is dressed up, fish is not a low-fat food and the high levels of cholesterol and saturated fat found in some fish foods make them an unhealthy option.
It could be argued that diets containing oily fish are associated with a lower risk of heart disease and stroke compared to diets rich in red meat and dairy foods. However, a vegetarian or vegan diet is the healthiest option. Dr Neal Barnard, president and founder of the Physicians Committee for Responsible Medicine in Washington DC, says that fish are not low enough in fat or cholesterol to achieve what vegetarian diets can in terms of promoting health. He points out that although the fat content of fish varies widely, all fish contain cholesterol and more fat than is generally found in the foods that make up a well-balanced plant-based diet (wholegrains, pulses, fruit and vegetables) most of which contain well under 10 per cent fat (Barnard, 2003).
In summary, plant-based diets inevitably contain considerably lower amounts of saturated fat (and either less or no cholesterol) compared to typical Western diets. Research shows that vegetarians consume a third less saturated fat and only half as much cholesterol as omnivores. Vegans consume even less: half the amount of saturated fat eaten by omnivores and no cholesterol (Davis and Kris-Etherton, 2003). This contributes significantly to their lower risk of heart disease, stroke and many other diseases.
Getting to know the EFAs:
In the late 1920s the scientists George and Mildred Burr first introduced the idea that specific components of fat could be necessary for normal growth and development (Burr and Burr, 1929). Since then two specific polyunsaturated fatty acids have been classified as ‘essential’ as they cannot be manufactured within the body; they must be provided in the diet. Hence, they are called ‘essential fatty acids’ (EFAs). The two EFAs required for good health are the omega-3 fatty acid alpha linolenic acid (ALA) and the omega-6 fatty acid linoleic acid (LA).
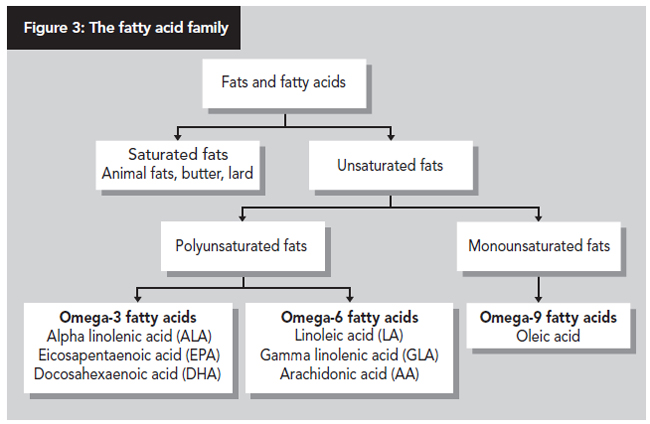
ALA is described as an omega-3 fatty acid because the first double bond occurs at the third carbon atom along the carbon backbone of the molecule. As shown in Figure 3, ALA can be converted in the body into the longer-chain omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). LA is an omega-6 fatty acid (as the first double bond occurs at the sixth carbon atom). Similarly, our tissues can convert it into other longer chain omega-6 fatty acids, such as gamma-linolenic acid (GLA) and arachidonic acid (AA).
Although AA, GLA, DHA and EPA are physiologically important, they are not referred to as ‘essential’ as they can be produced in the body from LA and ALA. The essentiality of ALA and LA in humans is best explained by our inability to introduce double bonds in positions before carbon nine (Uauy et al., 2003). In other words, they are classed as essential as we can’t make these fats in our bodies.
EFAs are important for the normal functioning of all tissues of the body. They are necessary for the formation of healthy cell membranes, the proper development and functioning of the brain and nervous system and for the production of eicosanoids, important regulators of vital body functions such as blood pressure, blood-clotting, and immune and inflammatory responses.
How much fat?
The UK Dietary Reference Values for the total amount of fat and different fatty acids in the diet were published in 1991 (Department of Health, 1991). Additional recommendations were made for omega-6 and omega-3s by the Committee on Medical Aspects of Food (COMA) in 1994 in a review on the nutritional aspects of CVD (COMA, 1994).
Taken together, current UK recommendations are that total fat intake should contribute no more than 33 per cent of daily total energy intake and that saturated fats should contribute an average of no more than 11 per cent of food energy, monounsaturated fats an average of 13 per cent, polyunsaturated fats 6.5 per cent and trans fats no more than two per cent. COMA recommended that among the general population there should be no further increase in average intakes of omega-6 fats but that intakes of long-chain omega-3 (EPA and DHA) fats should increase from about 0.1 grams to 0.2 grams per day (COMA, 1994).
These recommendations are similar to those given by the World Health Organisation (WHO) and Food and Agriculture Organisation (FAO). These are summarised along with the actual amounts of each type of fat required to meet these recommendations in Table 2.
Table 2: WHO recommendations for daily fat intake
| Type of fat | Percentage of total energy | Grams required for women (aged 19-50) consuming 1,940 calories/day | Grams required for men (aged 19-50) consuming 2,550 calories/day |
|---|---|---|---|
| Total fat | 15-30 | 32.3-64.7 | 42.5-85.0 |
| Saturated fat | Less than 10 | Less than 21.6 | Less than 28.3 |
| Polyunsaturated fats | 6-10 | 13.0-21.6 | 13.3-28.3 |
| Omega-6 | 5-8 | 10.8-17.2 | 14.2-22.7 |
| Omega-3 | 1-2 | 2.2-4.3 | 2.8-5.7 |
In summary, total fat intake should contribute between 15-30 per cent of total energy intake with less than 10 per cent from saturated fat. Those obtaining more than 10 per cent of their dietary energy from omega-6 fats should not increase their intake of this fat. Most people need to increase their intake of omega-3s to provide two per cent of dietary energy. Less than one per cent of calories (but preferably none), should come from trans fats.
Oily fish have fats throughout their whole body rather than only in the liver like non-oily (white) fish. Oily fish fillets may contain up to 30 per cent fat, although this figure varies both within and between species. See table 3 for a list of oily and non-oily fish.
How much oily fish?
In 2004, in response to a specially commissioned report on the benefits and risks of oily fish consumption, the Food Standards Agency (FSA) issued guidelines on oily fish intake. Table 4 shows the recommended weekly limits. They suggest a limit on the maximum number of portions of oily fish different groups can safely consume each week (a portion is about 140 grams). However, the FSA says that health benefits are greater than the risks as long as you don’t eat more than the recommended maximums. Hardly reassuring!
EFA deficiency
For EFA deficiency to develop, dietary intake must be extremely low as even small amounts of EFAs can prevent deficiency. The 2003 National Diet and Nutrition Survey showed that the average daily total fat intakes were close to UK recommendations (FSA, 2003). In fact, most adult Western diets provide 8-15 grams of EFAs per day and healthy people have a body reserve of 500-1000 grams in adipose tissue (Department of Health, 1991). EFA deficiency in adults is only seen when they make up less than 1-2 per cent of total dietary energy (Department of Health, 1991). Where EFA deficiency does occur, it is most often seen in infants fed very poor diets.
Typical symptoms of EFA deficiency include excessive thirst, frequent urination, dry or rough skin, dry hair, dandruff, brittle nails, headaches, stomach ache, diarrhoea and constipation (Stevens et al., 1995). Low omega-3 fatty acid status is also associated with behavioural problems such as hyperactivity-impulsivity, anxiety, temper tantrums, sleep problems and learning difficulties in some children (Stevens et al., 1996). More specifically, low levels of DHA have been associated with several neurological and behavioural disorders such as depression, schizophrenia, Alzheimer’s disease and attention deficit hyperactivity disorder (ADHD) (Davis and Kris-Etherton, 2003).
These findings are consistent with evidence that omega-3 fatty acids are important for brain function and that low omega-3 intake may have negative effects on behaviour, learning and mood. It is important then to make sure that there are adequate levels of these important nutrients by supplying sufficient ‘parent’ fatty acids for conversion. Most people can obtain all the EFAs they require from a well-balanced plant-based diet including flaxseed oil, nuts and seeds as well as plenty of green leafy vegetables. In most cases, dietary replenishment of EFAs will usually reverse any deficiency.
Table 4: UK Food Standards Agency recommended limits for oily fish per week
| Two portions | Four portions |
|---|---|
| Women who are pregnant or breastfeeding and girls and women who might have a baby one day | Other women and men and boys |
Table 5 shows which plant-based foods can be used to boost your intake of omega-3 fats. Note that the fats and oils are easily damaged by light or heat so are best kept refrigerated. Furthermore, these oils should not be used in cooking; use them on salads, in dressings and dips.
Table 5: Plant sources of EFAs
| Food oils | Omega-3, ALA g/100g | Omega-6, LA g/100g |
|---|---|---|
| Flaxseed (linseed) oil | 53.30 | 12.70 |
| Hempseed oil * | 20.00 | 60.00 |
| Walnut oil | 10.40 | 52.90 |
| Rapeseed (canola) oil | 9.13 | 18.64 |
| Wheat germ oil | 6.90 | 54.80 |
| Soya oil | 6.79 | 50.42 |
| Corn oil | 1.16 | 53.23 |
| Sunflower oil | 0.00 | 65.70 |
| Nuts and seeds | Omega-3, ALA g/100g | Omega-6, LA g/100g |
|---|---|---|
| Flaxseeds (linseeds), ground | 22.81 | 5.90 |
| Walnuts | 9.08 | 38.09 |
| Hempseeds * | 7.50 | 22.50 |
| Vegetables, Fruits and Pulses | Omega-3, ALA g/100g | Omega-6, LA g/100g |
|---|---|---|
| Soya beans, cooked | 0.60 | 4.47 |
| Tofu firm | 0.58 | 4.34 |
| Broccoli (cooked) | 0.11 | 0.05 |
| Soya milk | 0.08 | 0.59 |
| Strawberries | 0.07 | 0.09 |
| Peas (frozen and cooked) | 0.02 | 0.08 |
* Adapted from Leizer et al., 2000.
People with diarrhoea, irritable bowel syndrome, diverticulitis or inflammatory bowel disease (Crohn’s disease or ulcerative colitis) should use caution if taking flaxseed (but not flaxseed oil) due to its possible laxative effects. If you have a medical condition, or are taking other drugs or supplements you should consult a doctor or nutritional therapist before changing your diet.
Balancing the fat
Research suggests that the ratio of omega-6 to omega-3 fatty may be more important than the amounts of individual fatty acids consumed (Lands, 1992). This is because omega-6 fats compete with omega-3s for use within the body. So excessive intakes of omega-6 fats can cancel out the positive effects of omega-3s and lead to health problems.
Recent changes in the diet have led to a massive rise in our intake of omega-6 fats from plant-based oils (such as sunflower oil) and most processed foods. This has increased the ratio of omega-6 to omega-3 fats in our diets.
Typical Western diets may provide ratios of up to 30:1, dramatically skewed toward omega-6 fats. The health consequences of this could be far-reaching. Dr. Hibbeln, lead clinical investigator on nutrition in psychiatry at the National Institutes of Health in Bethesda, Maryland suggests that these major changes in the essential fatty acid composition of the food supply may be linked to a range of psychiatric disorders and may even contribute towards an increased risk of homicide, suicide and social instability (Hibbeln, 2007).
The WHO/FAO joint recommendation is a ratio of LA to ALA of 5:1-10:1 (WHO/FAO, 1994). Other recommended ratios vary but a cautious approach would be to aim for a ratio between 2:1 and 4:1 making sure not to exceed 6:1 (Davis and Kris-Etherton, 2003). This ratio can be achieved by reducing the use of sunflower, safflower and corn oils and increasing the use of ALA-containing oils such as flaxseed, rapeseed and soya bean oils. Of course, optimising omega-3 conversion rates can help improve your omega-6:omega-3 ratio too.
Optimising conversion
The body converts ALA into the longer chain omega-3s (EPA and DHA), otherwise found in fish and some species of algae. However, we are repeatedly told (particularly by fish oil supplement companies) that conversion rates are low and inefficient. The claim that we cannot convert enough ALA to EPA and DHA is simply not true, but does serve to protect the fish oil market. The better health statistics for vegetarians and vegans – who don’t eat fish – provides proof that they don’t go short.
Several studies have measured the rate at which we convert ALA to EPA and DHA. A conservative estimate is that about 5-10 per cent of ALA is converted to EPA, and 2-5 per cent to DHA (Davis and Kris-Etherton, 2003). However, as the body’s fat deposits usually contain ALA, even a very low conversion rate of just 2.7 per cent, would allow an average person to make the same amount of EPA as would be found in 18 large (1,000mg) capsules of the omega-3 richest fish oil (Erasmus, 1993). Even a person with no omega-3 fats in their body, (perhaps after a long-term dietary shortfall) who takes two tablespoons of flaxseed oil a day, can produce more EPA than contained in two large fish oil capsules.
Other studies show much higher levels of conversion. Research from the Institute of Human Nutrition at the University of Southampton found ALA conversion rates in young women of 21 and nine per cent for EPA and DHA respectively (Burdge and Wooton, 2003).
Furthermore, a recent study from the University of Cambridge revealed that vegetarians convert more ALA to EPA and DHA than fish-eaters (Welch et al., 2008). In this study, the ratio of circulating EPA and DHA to dietary intake of ALA was used as an indicator of conversion rate; the higher the ratio, the greater the conversion rate. Results showed the ratio was 22 per cent higher in vegetarians than fish-eaters, indicating a higher conversion rate. This may explain why fish-eaters and non fish-eaters have a smaller than expected difference in circulating omega-3 levels.
Taken together, the research indicates that we can convert as much or as little as we need, providing we have enough starting material (ALA).
In addition to this, we are capable of ‘retroconversion’, which means we can make EPA from DHA. Research from the Department of Nutritional Sciences at Pennsylvania State University states that up to 10-11 per cent of DHA is retroconverted to EPA. The authors of this study conclude that if sufficient ALA and DHA are consumed, total EPA production would be expected to be adequate (Davis and Kris-Etherton, 2003).
So if you take an algal supplement that contains DHA you can boost both DHA and EPA levels without exposing yourself to toxic pollutants found in fish oils. Furthermore, the EPA we make in our bodies has the advantage of being fresher and more stable than that found in fish oils.
A range of dietary factors can affect efficiency of conversion too. Poorly designed diets are thought to reduce the rate of conversion as both energy and protein are needed to drive the enzymes that convert EFAs. In addition, a wide range of nutrients are required to optimise conversion including biotin, calcium, copper, magnesium, niacin (vitamin B3), pyridoxine (vitamin B6), vitamin C and zinc (McKevith, 2005; Siguel and Lerman, 1994; Horrobin, 1992). A well-balanced plant-based diet will provide all these nutrients and more.
Excessive intakes of trans fatty acids can limit conversion rates. These unhealthy fats, found in hydrogenated fat in margarine and products made with it (such as biscuits and pastries), are also found in meat and dairy products. Alcohol inhibits activity of the enzymes that convert ALA into EPA and DHA and depletes tissues of these long chain omega-3 fatty acids (Davis and Kris-Etherton, 2003).
Consuming excessive amounts of omega-6 fatty acids (associated with some vegetable oils, particularly safflower, sunflower and corn oils) can have a detrimental effect on conversion rates too (Uauy and Castillo, 2003). Indeed, a high omega-6 intake may reduce omega-3 conversion by as much as 40 per cent (Davis and Kris-Etherton, 2003). There is no need to avoid or cut down on omega-6-rich wholefoods (sunflower seeds, pumpkin seeds, sesame seeds, wheat germ and soya foods) as they contribute much less to overall omega-6 intake and contain an abundance of other healthy nutrients.
Davis and Kris-Etherton recommend that the primary fat in the diet should come from foods and oils rich in monounsaturated fat, as when monounsaturated fats predominate, saturated fats, trans fats and omega-6 fats are kept in check (Davis and Kris-Etherington, 2003). Monounsaturated fats are found in nuts, peanuts, olives and olive oil, avocados and rapeseed oil. As stated, wholefoods are superior source of fats as they contribute many other nutrients to the diet.
Lastly, it is important to optimise the intake of ALA for conversion into EPA and DHA. As stated above, ALA should provide 1-2 per cent of total energy intake in the diet. Good sources include ground flaxseeds and their oil, hempseed, rapeseed, walnuts, soya beans and products made from them, green leafy vegetables and some species of algae (which contain DHA). Table 6 shows the amount of omega-3-rich food you can take to achieve the recommended daily intake (along with a well-balanced plant-based diet).
Table 6: Suggested daily intake of foods rich in omega-3
| Source | One of the following |
|---|---|
| Flaxseed (linseed) oil | 1-2 tsp |
| Ground flaxseed | 2 tbsp |
| Rapeseed oil | 2 tbsp |
| Hempseed oil | 1 tbsp |
| Walnuts | 8 halves (28 grams) |
If more people knew that they could produce sufficient amounts of EPA and DHA from ALA they might be less inclined to turn to potentially decaying and contaminated fish oils. The research indicates that the only thing vegetarians and vegans miss out on by avoiding fish is the toxic pollutants that contaminate them.
Omega-3s from algae – cut out the middleman
Whilst omega-3 is present in fish oil, fish do not produce omega-3 in their bodies. Fish obtain their omega-3 from their diet of algae. People who are concerned about intake of DHA can use algal supplements as a source of this long chain omega-3 too. There are even brands available online that can provide both DHA and EPA.
Algae used for omega-3 supplements is usually grown in controlled conditions away from the sea, so it doesn’t interfere with the marine ecosystem and doesn’t impact on fish stocks nor their natural food source. So, in addition to the numerous health benefits of this vegan-friendly source of long chain omega-3s, it is a more environmentally friendly choice.
By switching from fish to a plant-based source of omega-3 you’ll be doing yourself a favour and the environment too, whilst getting the safest, toxin-free omega-3 fats.
Heart health
Why are oily fish promoted as essential for good health? The answer lies, partly, in the role EFAs may have in lowering the risk of heart disease and stroke.
Oily fish first got the nutritional thumbs up when it was observed that populations such as the Japanese and Inuit (Eskimo) people, with their fish-rich diets, have much lower rates of CVD. Further investigation suggested that the EPA and DHA fatty acids found in fish can help reduce blood-clotting, lower blood pressure and cholesterol levels and lower triglyceride (fat) levels in the body. All these effects can help lower the risk of CVD. However, the promotion of oily fish ignores the fact that EPA and DHA can also be formed within the body from plant sources of ALA. Not to mention the toxic pollutants found in fish and the environmental catastrophe of industrial fishing.
Numerous studies have looked at the benefits of eating polyunsaturated fatty acids (particularly the omega-3s: ALA, EPA and/or DHA) to reduce the risk of heart disease. Three major studies are frequently referred to: the DART, GISSI and LYON studies. The DART and GISSI trials demonstrated how fish oils could reduce mortality in people with CVD. However, there is now a large body of evidence showing how plant-based ALA can do the same without exposure to harmful toxins found in oily fish. The third well-known study, the LYON study, clearly demonstrated this.
DART – using dietary fish to prevent secondary heart disease
One of the best-known early studies was the Diet and Reinfarcation Trial (DART) (Burr et al., 1989). This study looked at the effects of dietary intervention in the secondary prevention of heart attacks in patients who had previously recovered from one. In this study 2,033 men who had recovered from a heart attack were allocated to receive or not receive advice to eat around 300 grams of oily fish per week, or take fish oil supplements giving an equivalent amount of omega-3 fats.
Results showed that the fish group had a 29 per cent reduction in death during the two year recovery period following a heart attack. So it was concluded that fish oil may reduce CVD mortality; the effect being greatest during the period of recovery following a heart attack.
Burr suggested that omega-3 fats may help normalise heartbeat rhythms by exerting what is called a beneficial anti-arrhythmic effect. In other words, omega-3s may help your heart beat more regularly and calm irregular activity (arrhythmia). Others agree that the most likely mechanism by which EPA and DHA reduce the recurrence of heart disease is by stabilising arrhythmias (Marchiolo et al., 2002). Research suggests that the anti-arrhythmic effect of omega-3 fats is partly due to their ability to reduce the electrical excitability of cells.
As stated, fish oils (or components of them) may also offer benefit by reducing blood-clotting. Platelet cells found in the blood ensure that blood becomes sticky (platelet aggregation or blood-clotting). This is important for stopping bleeding, for instance, if you are wounded. However, too much clotting can cause the cells to clump together and stick to the walls of blood vessels. This can lead to heart disease and stroke. EPA appears to reduce the tendency of blood platelets to clump together. Consequently, it may prevent the formation of blood clots and the narrowing of coronary arteries, which can lead to a heart attack. However, extensive reduction in platelet aggregation can lead to prolonged bleeding times following injury. It is important that blood is neither too thick nor too thin.
Those taking blood-thinning medication (such as daily aspirin or warfarin), should speak to their GP before eating lots of food that has added omega-3 or before taking fish oil supplements, as this can also reduce blood-clotting.
Interestingly, although there were less fatal heart attacks among the DART fish group, the total number of attacks was not reduced. So although eating oily fish reduced the risk of dying after a heart attack, it did not prevent a secondary heart attack. Whereas a large body of evidence shows that plant-based diets can be used to both prevent and even reverse heart disease (see the guide Have a Heart for further information).
GISSI – using fish oil supplements to prevent secondary heart disease
The GISSI-Prevenzione trial similarly looked at the effect of EPA and DHA on 11,324 patients (primarily men) who had recently survived a heart attack. Half the participants received a daily supplement (1 gram per day) of omega-3 fish oil capsules, while the other half did not (GISSI, 1999).
After three-and-a-half years, results showed a 20 per cent reduction in the overall death rate among the fish oil group. However, like the DART trial, the rate of non-fatal heart attacks was unchanged. It should also be noted that the large amount of omega-3 fats given (1 gram) is the equivalent of consuming a very large amount (around 100 grams) of oily fish per day. This exceeds the ‘safe’ amount the UK government recommends (FSA, 2009).
More recently, a Finnish study looking at the relationship between omega-3 levels and the five-year risk of heart attack and death in patients with heart disease found that relatively high blood levels of omega-3 fats were associated with a lower risk of death (Erkkilä et al., 2003). However, like the previous trials, omega-3s did not prevent the recurrence of a heart attack. This finding fits well with those from earlier studies showing that fish consumption and omega-3s may be associated with decreased death rates but do not necessarily prevent a secondary heart attack in high-risk subjects. Conversely, there is a huge body of evidence (see below) showing how vegetarian or vegan diets can actually reverse heart disease in patients and so reduce both death rates and secondary heart attacks.
No benefit from fish for low-risk heart disease populations
While the DART and GISSI trials suggested that fish oils may reduce death rates in people who have already had a heart attack, the same cannot be said for the wider population. A major review of studies examining the relationship between fish intake and heart disease found that fish consumption is not associated with a reduced risk in low-risk populations (people with no history of heart problems) (Marckmann and Gronbaek, 1999). This review concluded that healthy people (at low-risk of heart disease) do not gain any additional protection for the heart from eating fish. The authors question whether the apparent protection in high-risk individuals is attributable to eating fish or whether the link might be explained by other dietary or non-dietary confounding factors.
In a later editorial, one of the review authors reaffirmed that while an average daily intake of 50 grams of fish may lower heart disease death rate, the apparent protection is limited to high-risk populations (Marckmann, 2003). Marckmann observes that both the DART and GISSI trials were well-designed and performed and the results were convincing. However, he says that their conclusion, that heart disease patients should be prescribed oily fish or fish oil supplements, has been seriously challenged by more recent research.
No long-term protection against heart disease
A long-term follow-up to the DART study (Ness et al., 2002), showed that the death rate in the two groups (fish and no fish) after an average follow-up of 15 years was almost identical. So the dietary advice given to former DART participants, over a decade previously, offered no long-term protective effect. So while fish oil may offer short-term protection to people who have suffered a heart attack, this protection does not appear to stand the test of time.
A further study looked at whether dietary advice (to eat oily fish or fish oil supplements) could reduce the death rate among men with angina (Burr et al, 2003). Another surprising result was found: advice to consume fish and the intake of fish oil capsules was associated with an increase in mortality of 20 per cent and 45 per cent respectively! Furthermore, this increase was even more prominent for sudden death. Such results should make health organisations and the Government sit up and rethink their position on fish and fish oil in the primary and secondary prevention of heart disease.
More recently, in 2006, a major review published in the British Medical Journal drew the evidence together by reviewing all the relevant studies published over the previous four years (Hooper et al., 2006). It looked at 89 studies on omega-3 fats and health and concluded that long chain and shorter chain omega-3 fats do not have a clear effect on total mortality, combined cardiovascular events or cancer.
The review noted that the 2003 study by Burr contradicts the other large studies by not suggesting a benefit of omega-3s in patients with angina. One possible explanation the researchers suggest for this is that as this trial had the longest follow-up period of all the studies reviewed it could be that the negative effects of oily fish and fish oil supplements were due to the cumulative harmful effects of mercury. In other words, the pollutants in fish and fish oil supplements taken over time may cancel out the beneficial effects of the omega-3 fats they contain.
Another study found fish oil supplements increased life-threatening abnormal heart rhythms in patients with implanted defibrillators (Raitt et al., 2005). This study actually found that fish oil supplementation did not reduce the risk of abnormal or irregular heart rhythm and may even be pro-arrhythmic in some patients.
LYON – using plant-derived ALA to prevent secondary heart disease
The Lyon Diet Heart Study investigated whether a Mediterranean-type diet could reduce secondary heart disease (a second heart attack) compared to a prudent Western-type diet (de Lorgeril et al., 1999).
In this study, 423 patients with a history of heart attack were randomly assigned either a Mediterranean diet or a prudent Western diet (as recommended by the American Heart Association). The Mediterranean diet was largely plant-based containing more bread, pulses (peas, beans and lentils), vegetables (both root and green vegetables) and fruit. Butter and cream were replaced with healthier fats including olive oil and rapeseed oil margarine. The diet did contain fish, but less red meat, and overall it was lower in animal fat.
The Mediterranean diet was significantly lower in cholesterol and higher in a number of beneficial substances such as ALA. Earlier work with this group revealed a 70 per cent increase in circulating levels of ALA and a 40 per cent rise in EPA (de Lorgeril et al., 1994). Although fish intake was encouraged, the experimental group ate only seven grams a day more fish than the control group, leading the researchers to conclude that the favourable EPA level seen in the test group was due to plant-ALA intake rather than the fish in the diet.
Results showed a striking drop in death rates (due to a reduction in heart disease) of close to 70 per cent. Compared with the DART trial, the protective effect was associated with ALA instead of EPA. Another important difference was that the protection ALA offered extended to non-fatal heart attacks. The authors of this study suggested that moderate amounts of omega-3 fatty acids (such as in the Mediterranean diet), may work in multiple ways to reduce the risk of heart attacks and sudden death.
Just to be clear, the only fatty acid associated with the reduction in heart attacks was ALA. The authors did not find any correlation between the longer-chain omega-3 fatty acids (EPA and DHA) and a reduction in cardiac events. The Lyon Diet Heart Study demonstrated that plant-derived ALA is extremely effective in reducing the risks of secondary heart disease. It demonstrated that plant ALA was superior to fish-derived EPA and DHA in reducing the risk of a second heart attack. This study also confirmed that ALA can confer long-term protection to heart health.
Three years later, in an article published in the journal Circulation, Dr J. David Spence of the Stroke Prevention and Atherosclerosis Research Centre at Robarts Research Institute in London, Canada, asked why the Lyon study was so neglected (Spence, 2002). Spence believes this study should have set the benchmark for dietary recommendations. He stressed how Mediterranean diets have been shown to improve endothelial function (how the internal lining of the blood vessels work). Spence also attributed the protective role of this type of diet to the higher levels of antioxidants they contain. A large body of evidence indicates that antioxidants may be able to reduce atherosclerosis (the progressive thickening and hardening of arterial walls that results from the build up of fatty deposits) (Azen et al., 1996).
Spence also suggested that dietary cholesterol is more harmful to health than previously thought. Cholesterol is a fatty substance mainly produced by the liver (in response to saturated fat intake) but it is also supplied in diets containing animal-based foods (meat and dairy). Plant foods don’t contain any cholesterol. It is carried in the bloodstream by molecules called lipoproteins (a mixture of fat and protein). Low-density lipoprotein (LDL) takes cholesterol from the liver to the cells and is often referred to as ‘bad’ cholesterol because when levels are high, it can accumulate on the walls of the arteries. High-density lipoprotein (HDL) carries excess cholesterol back to the liver for excretion and is therefore called ‘good’ cholesterol.
Evidence suggests that LDL can also harm the walls of the arteries when it is damaged or oxidised (Galassetti and Pontello, 2006). So what has this to with the diet and what can be done about it? Well, quite a lot. For example, one study showed how eating two eggs a day for three weeks not only raised LDL levels by about 10 per cent but increased oxidised LDL by 34 per cent (Levy et al., 1996). The authors concluded that egg consumption, in addition to raising cholesterol, increased how readily LDL could be oxidised. This, in turn, enhanced the progression of atherosclerosis (the build up of fatty deposits in the arteries). It was concluded that this may contribute to the high levels of heart disease seen in populations with high cholesterol intakes.
The precise mechanism underlying how eggs increase LDL oxidation is unclear, although their relatively high omega-6 intake has been blamed (Shapira and Pinchasov, 2008). Conversely, a healthier diet, such as the Mediterranean diet (rich in antioxidants and flavanoids), appears to reduce how readily LDL is oxidised (Lapointe et al., 2006). Interestingly though, antioxidant supplements and fish oil supplements have not been clearly demonstrated to prevent LDL oxidation.
Research shows that LDL in vegetarians is less susceptible to oxidative damage (Lu et al., 2000). This may be due to the low-fat, high-antioxidant (beta-carotene and vitamins C and E) and/or soya food content of a well-balanced plant-based diet. This could be one of the reasons why the Mediterranean diet is associated with a lower incidence of heart disease (Lapointe et al., 2006). These and other studies provide strong evidence that plant-based omega-3s can protect heart health and that contrary to popular belief, oily fish are not the only (nor indeed the best) source of these valuable nutrients.
Spence states that it is no longer reasonable for patients with heart disease to be prescribed diets containing a daily intake of animal flesh (Spence, 2002). Dietary recommendations, he suggests, should be based on diets similar to that used in the Lyon study.
Plant omega-3s and heart disease
Many other studies indicate that plant omega-3s have a protective effect against heart disease. The Health Professionals’ Study looked at 43,757 men over six years (Ascherio et al., 1996). During this time 229 men suffered a fatal heart attack and 505 a non-fatal heart attack. This study found that a one per cent increase in ALA intake lowered the risk of heart attack by 59 per cent. It was concluded that diets high in ALA from plants are associated with a reduced risk of heart disease.
Similar findings were reported in the Nurses’ Health Study which looked at over 76,000 women over 10 years (Hu et al., 1999). During this time 232 women suffered a fatal heart attack and 597 a non-fatal attack. Those who consumed the most ALA had a 45 per cent lower risk of fatal heart disease. The risk was further lowered among women who also took vitamin E supplements or who had a lower intake of trans fatty acids. The authors concluded that higher consumption of foods such as oil-based salad dressings that provide polyunsaturated fats, including ALA, may reduce the risk of fatal heart disease.
In the 2001 National Heart, Lung and Blood Institute Family Heart Study, the diets of 4,584 participants were assessed (Djousse et al., 2001). Results showed that men who consumed the most ALA had a 40 per cent lower risk of heart disease and women who consumed the most had a whopping 50-70 per cent reduction.
In 2003, a joint report by WHO/FAO concurred that ALA has a protective effect against heart disease (WHO/FAO, 2003). The report states that several prospective studies have found an inverse association between the intake of ALA (from flaxseed, rapeseed and soya bean oils) and risk of fatal heart disease. In other words, ALA protects against death from heart disease.
It has been suggested that the protective effects of ALA are particularly evident among subjects with low intakes. This may be in parts of Europewhere sunflower oil is used almost exclusively, or in developing countries where palm oil is used (both oils lack ALA).
In 2008, a study published in Circulation, the Journal of the American Heart Association, investigated the role of ALA in heart disease in Costa Rica where ALA intake was low but is increasing due to the switch from palm oil to soya bean oil (Campos et al., 2008). This study found that a 1.79 gram per day intake of (supplying 0.65 per cent of total energy) decreased the risk of a second heart attack in heart disease patients by 57 per cent, compared to a 1.11 gram per day intake (supplying 0.42 per cent of total energy). The authors suggest that the amount of ALA needed to reduce the risk of a second heart attack can be obtained from just 2 teaspoons of soya bean or rapeseed oil, 1-2 millilitres of flaxseed oil or just 6-10 halves of walnuts per day.
The Cochrane Collaboration is an international not-for-profit, independent organisation, dedicated to making up-to-date, accurate information about the effects of healthcare readily available worldwide. The Collaboration’s systematic reviews of healthcare studies are published quarterly as part of The Cochrane Library. Cochrane reviews have become known internationally as sources of high quality, reliable health information.
In 2004, the Cochrane Collaboration reviewed the current evidence to see whether dietary or supplemental omega-3 fatty acids alter total mortality (death rate) or cardiovascular events (heart attack and stroke) (Hooper et al., 2004). They concluded that there was no overall benefit either on heart attacks, deaths from heart disease or overall mortality. The authors concluded that there was not enough evidence to say that people should stop taking rich sources of omega-3 fats, but said that further high quality trials are needed to confirm the previously suggested protective effect of omega-3 fats for those at increased cardiovascular risk.
With declining fish stocks, polluted seas and oceans, the role of plant-based omega-3s in heart disease must be further examined. The possibility of a simple and sustainable plant-based solution can no longer be ignored.
Veggie diets and heart disease
Plant-based diets have been shown to prevent and even reverse heart disease. Dr Dean Ornish, Clinical Professor of Medicine at the University of California in San Francisco, is well-known for his Lifestyle Heart Trial in which he treated severe heart disease patients with lifestyle changes alone (Ornish et al., 1990; Ornish et al., 1998). The experimental group ate a low-fat wholegrain plant-based diet containing lots of fruits, vegetables and pulses. They also followed an exercise programme, practised various forms of stress management but did not receive medication. They were monitored against a control group of similar patients who received conventional treatments.
After just one year, 82 per cent of patients on this lifestyle change regime had regression of their heart disease with a 91 per cent reduction in chest pain and reduced cholesterol levels. Whereas the control group experienced a 165 per cent increase in the frequency of chest pain, cholesterol was worse and blockages of their arteries became worse. This trial has continued with similar results and continues to achieve better results than conventional surgical or medical intervention.
More recent work shows that vegetarians generally have a much lower risk of heart disease than meat-eaters. A major review of the scientific evidence shows that vegetarians have a massive 25 per cent lower risk of dying from heart disease! The authors of this study conclude that the widespread adoption of a vegetarian diet could prevent approximately 40,000 deaths from heart disease in Britain each year (Key et al., 1999).
As stated, meat, poultry, fish, eggs and dairy products all contain cholesterol, while a plant-based diet contains little or no cholesterol. It should be no surprise then that a large-scale study investigating cholesterol levels among vegans, vegetarians, fish- and meat-eaters found that the vegans had the lowest levels, vegetarians and fish-eaters had similar values and the meat-eaters had the highest (Appleby et al., 1999).
For vegans it’s a win-win situation. Not only do they avoid harmful substances (saturated animal fat, animal protein and cholesterol), they also benefit from a wide range of healthy nutrients including fibre, vitamins and minerals.
Inflammatory diseases
It is reported that omega-3 fats can help fight heart disease, asthma, type 1 diabetes and multiple sclerosis. The beneficial effects have also been seen in some cancers, inflammatory bowel disease, arthritis, osteoporosis, mental health, dry eye disease, age-related macular degeneration and psoriasis (Simopoulos, 2008). Many of theses conditions involve inflammation.
Our bodies use inflammation to protect tissues from infection, injury or disease. The inflammatory process usually promotes healing but, when uncontrolled, it can also harm. We now know that the balance of omega-6s to omega-3s is important for regulating inflammation. As a general rule, omega-6 fats are thought to be pro-inflammatory, whereas omega-3 fats are considered anti-inflammatory (GLA is the exception as it is an omega-6 fat with anti-inflammatory properties). The dramatic increase in dietary saturated and omega-6 fats, coupled to the decrease in omega-3 fats is linked to the increasing incidence of numerous inflammatory diseases including asthma, allergy and atherosclerosis (Chilton et al., 2008).
There is evidence that changing the diet can help some people with inflammatory conditions; some of these are discussed below.
Arthritis
Arthritis is a painful condition of the joints and bones. There are many different forms of this condition. The two main types are rheumatoid arthritis and osteoarthritis. Other forms of arthritis include ankylosing spondylitis, cervical spondylitis, fibromyalgia, lupus, gout, psoriatic arthritis and Reiter’s syndrome (NHS Direct, 2008).
Osteoarthritis
Osteoarthritis is the most common type of arthritis in the UK, with an estimated 8.5 million people affected by the condition (NHS Direct, 2008a). This degenerative disease is sometimes referred to as ‘wear and tear’ arthritis. Cartilage is the strong, smooth surface that lines the bones and allows joints to move against each other easily without friction. In osteoarthritis, cartilage gradually breaks down faster than it can be repaired. Eventually the surface of the bones begin to rub together causing them to degenerate.
In osteoarthritis, damage to cartilage can result in bony growths developing around the edge of the joints causing mild inflammation of the tissues (synovitis). Osteoarthritis mostly occurs in the knees, hips and small joints of the hands. However, almost any joint can be affected.
Osteoarthritis generally occurs in the over 50s and is more common in women than men. However, it is not an inevitable part of getting older. It can develop after an injury to a joint; this can happen months or even years after the injury.
Studies have been carried out to try to find whether omega-3 fats and/or fish oils can be helpful for osteoarthritis, but the results so far are inconclusive.
Rheumatoid arthritis
Rheumatoid (inflammatory) arthritis is a more aggressive, but less common condition than osteoarthritis. It is thought to be an autoimmune disease whereby the body’s own immune system attacks the joints, causing pain, swelling and the destruction of bone and cartilage.
This chronic condition is characterised by hot painful swelling in the joints. It usually starts in the wrists, hands and feet but can spread to other joints in the body. In some diseases inflammation can help towards healing, but in rheumatoid arthritis it tends to cause damage. For some people the discomfort, pain and loss of mobility caused by this condition can have a serious impact on their lives.
Rheumatoid arthritis affects approximately 350,000 people in the UK and like osteoarthritis, is also more common in women than men. It is most common after the age of 40, but can affect people of any age (NHS Direct, 2008b).
Diet and arthritis
In the past, arthritis patients were told that dietary changes would not help them. Despite this many arthritis patients have found that certain foods can worsen their condition, or improve it.
Arthritis Care is the UK’s largest voluntary organisation working with and for people with arthritis. It suggests that a diet high in fruit, vegetables, pasta, fish and white meat, and low in fatty foods such as red meat, cream and cheese can help (Arthritis Care, 2008). Most people would benefit from eating less saturated fat and sugar and eating more complex carbohydrates, fibre, vitamins and minerals. Evidence shows that at least for some people with arthritis, a healthier diet can help considerably.
In 2001, the first controlled study examining the long-term effect of a vegan, gluten-free diet on rheumatoid arthritis found that this diet could improve the signs and symptoms of this condition (Hafström et al., 2001). The authors of this study suggested that a gluten-free vegan diet may, in some people, reduce the immune response that triggers rheumatoid arthritis. Another study tested a low-fat, vegan diet in patients with moderate-to-severe rheumatoid arthritis (McDougall et al., 2002). Results also showed those who switched to this type of diet experienced a significant reduction in symptoms.
A further study showed that an uncooked vegan diet, rich in antioxidants and fibre, decreased joint stiffness and pain in patients with rheumatoid arthritis (Hänninen et al., 2000). Some studies have looked at fasting followed by a vegetarian or vegan diet. A review of these studies concluded that this dietary treatment might also be beneficial for people with rheumatoid arthritis (Müller et al., 2001). Taken together, these studies provide strong evidence that dietary modification can benefit arthritis patients.
Weight control
It is widely accepted that it is important for people with arthritis to maintain a healthy weight. The extra burden on the joints, in overweight or obese arthritis patients, can make symptoms considerably worse and losing weight can have a dramatic beneficial effect.
The Arthritis Research Campaign (ARC) promotes medical research into the cause, treatment and cure of arthritic conditions. ARC’s dietary guidelines for people with arthritis suggest that one of the most important links between diet and arthritis is being overweight (ARC, 2006).
Adopting a plant-based based diet can help people lose weight and maintain a healthy body weight. Numerous studies show that vegetarians and vegans weigh less than meat-eaters. A study of over 55,000 Swedish women revealed that the vegetarian and vegan women were less likely to be overweight or obese than the meat-eaters (Newby et al., 2005). In another study, the effects of a low-fat, plant-based diet on 64 overweight postmenopausal women was compared to a diet based on National Cholesterol Education Program guidelines (Barnard et al., 2005). Results showed that the low-fat, vegan diet was associated with significant weight loss. A subsequent review of 40 studies revealed that, on average, vegetarians and vegans weigh between six pounds and two stones less than meat-eaters (Berkow and Bernard, 2006).
When trying to lose weight, it is important to maintain a good intake of nutrients. A healthy balanced diet containing plenty of fruit and vegetables, pulses and wholegrain foods (wholemeal bread, brown rice and wholemeal pasta) provides a good supply of vitamins, minerals and fibre. A diet lacking in these foods and rich in meat, dairy and processed foods (such as white bread, white rice and white pasta) does not provide such a good source of nutrients. Find out how to achieve and maintain a healthy weight while protecting your health too in the V-Plan Diet guide.
Getting the fats right
ARC states that vegetarian diets have been shown to be helpful in the long-term to some people with rheumatoid arthritis. It also says that a vegan diet (no meat, fish or other animal products such as eggs, milk, cheese or other dairy products) may also be helpful (ARC, 2006). Conversely, studies have shown that people who eat large amounts of red meat seem to have a higher risk of developing inflammatory arthritis.
The key point here is that not only is a plant-based diet helpful because it contains beneficial substances (antioxidants and omega-3 fats), but a typical Western diet, rich in meat, dairy and processed foods, is detrimental as it contains high levels of harmful substances such as saturated fat. This unhealthy type of fat tends to come from animal-based food (particularly meat, poultry and dairy products) and processed foods (cakes, pastry and biscuits). This unhealthy fat is the most important kind to avoid as it can increase pain and inflammation in arthritis (ARC, 2006).
Plant-based diets tend to contain considerably less saturated fat and more healthy polyunsaturated fats. The research suggests that polyunsaturated omega-3 fats may help some people with arthritis and other inflammatory conditions. The fact that people also tend to lose weight on a vegan diet contributes further to its beneficial effects.
Omega-6 fats do not appear to benefit people with arthritis. In fact they may increase inflammation by competing with omega-3s (ARC, 2006). Most people have diets which already contain more omega-6 fats than they need. If you have inflammatory arthritis, it may be helpful to replace some of the omega-6 fats (found in sunflower oil, corn oil and products made from them such as sunflower margarines) with omega-3 fats from flaxseed, hempseed and rapeseed oils and walnuts. Obtaining plant-based omega-3s from these sources will ensure you get this healthy fat without exposing your body to the harmful toxins found in oily fish.
Gout
ARC warns that people with gout should not consume oily fish. Gout is a type of arthritis caused by a high level of urate in the body which can crystallise in the joints and cause severe pain and inflammation. Urate is produced from purines, which are chemicals that result from the natural death of cells. Cutting down on foods which are high in purines may be helpful if you have gout. This is best done by replacing animal-based foods (especially meat and fish) with other sources of protein, such as pulses (peas, beans, and lentils). Other dietary measures for gout include losing weight (if you are overweight) and avoiding excessive alcohol consumption, which has been associated with gout for centuries (ARC, 2006).
Calcium
A well-balanced healthy diet can help you if you are taking strong drugs for arthritis. In fact, ARC states that if you are taking strong drugs for arthritis there is even more reason to eat a good diet as it can help to protect the body against some of the side-effects of the drugs. For example steroids, such as prednisolone, can cause osteoporosis, particularly if you stay on them for a long time. Plenty of calcium in your diet will help to reduce the risk (ARC, 2006).
Arthritis Care points out that people with rheumatoid arthritis are at increased risk of developing osteoporosis and agrees that ensuring an adequate calcium intake is very important (Arthritis Care, 2007). While cow’s milk and dairy products are indeed a source of calcium, they are not the best source. This is because they contain animal protein. Excessive amounts of animal protein can upset the acid balance within the body, which then takes calcium from the bones to neutralise the acid. Even the usually pro-dairy National Osteoporosis Society says: “It is a good idea to avoid too much protein, particularly animal protein such as meat and cheese,” (NOS, 2008). It is also a good idea to avoid too much salt, fizzy drinks and caffeine for the same reason.
Healthier sources of calcium include green leafy vegetables (broccoli, kale, spring greens, cabbage, parsley and watercress – but not spinach), dried fruits (figs and dates) nuts (almonds and Brazil nuts), seeds (sesame seeds and tahini – sesame seed paste), pulses (peas, beans, lentils and soya products such as calcium-set tofu and calcium-enriched soya milk). For more information on calcium see the fact sheet Boning up on Calcium.
Iron
Some arthritis sufferers may be concerned about their iron intake, particularly – they may be told – if they avoid eating red meat. This should not be a concern as the British Medical Association and the American Dietetic Association agree that vegetarians are no more likely to suffer from iron deficiency than meat-eaters (BMA, 1996; American Dietetic Association, 2003). Indeed one of the largest studies of vegetarians and vegans in the world (the EPIC Oxford cohort study) looked at over 33,883 meat-eaters, 18,840 vegetarians and 2,596 vegans and found that the vegans had the highest intake of iron, followed by the fish-eaters, vegetarians then the meat-eaters (Davey et al., 2003). Cow’s milk and dairy products are an extremely poor source of iron, containing hardly any, whereas pulses, dried fruits and dark leafy vegetables are all excellent sources. For more information on iron see the fact sheet Ironing out the Facts.
Antioxidant action
The antioxidant vitamins A, C and E are thought to protect against disease (and aging) by defending the body against attack from harmful molecules called free radicals. These damaging molecules are produced naturally as your body breaks down food, or as a result of exposure to harmful chemicals (including cigarette smoke) or radiation.
The damage caused by free radicals plays a role in many diseases including cancer and arthritis. A particular class of free radicals (called reactive oxygen species) can promote the inflammatory response that occurs in rheumatoid arthritis (Filippin, 2008). A molecular mechanism linking free radicals to inflammation has been proposed. It suggests that free radicals activate molecules called transcription factors (nuclear factor-kappa B or NF-?B). These then activate genes involved in inflammatory and/or autoimmune responses. In other words, free radicals can cause a sequence of events rather like a line of dominos falling down, which may lead to inflammatory arthritis.
There is some evidence that anti-rheumatic drugs may exert their therapeutic effects by acting as antioxidants. For example, non-steroidal anti-inflammatory drugs (NSAIDs) have been shown to act as free radical scavengers (Merry et al., 1991). This means they may protect against the harmful effects of free radicals by ‘mopping them up’. However, antioxidants may be more useful in preventing damage before it occurs, rather than treating an already inflamed joint.
Too much iron in the blood can encourage the production of free radicals (McCord, 2004). Unlike the non-haem iron we find in plant foods, haem iron in meat is absorbed into the body whether it is needed or not. Thus meat can supply an overload of iron (but no vitamin C and very little vitamin E). Conversely, vegetables and wholegrains foods can supply as much or as little iron as is required, as well as an abundance of protective antioxidant vitamins, fibre and other nutrients.
Omega-3s and arthritis
For some arthritis patients, omega-3 supplements may be helpful, for example a tablespoon of flaxseed oil twice a day (this exceeds the 1 teaspoon-a-day recommendation for normal consumption). If this is helpful, it may be a good idea to try to reduce your intake to the lowest effective dose.
Additional treatments
Some arthritis patients have benefited from taking a herbal remedy isolated from Rosa canina, a type of rose hip (Winther et al., 2005). In a randomised, double-blind, placebo-controlled trial, published in the Journal of Rheumatology, 82 per cent of patients reported a reduction in pain after just three weeks of active treatment with this herbal remedy. The authors of the study concluded that it could alleviate symptoms of osteoarthritis. In fact pain was reduced to such an extent that there was a significant decrease in the consumption of painkillers such as paracetemol, ibuprofen and NSAIDs. This compares favourably to glucosamine, currently the most popular supplement for joint health (Reginster et al., 2001; Matheson and Perry 2003).
Summary
Losing weight, eating a healthy plant-based diet that includes a good supply of omega-3 fatty acids (either though foods or supplements) can help reduce the symptoms of arthritis and may help some people reduce their medication (ARC, 2006).
Multiple sclerosis
In multiple sclerosis (MS), the protective sheath (called myelin) that surrounds the nerve fibres of the central nervous system becomes damaged. This process is called demyelination. Sclerosis means scarring and multiple refers to the many different sites at which the scarring may occur in the brain and spinal cord. Demyelination interferes with the messages that are sent between the brain and other parts of the body. Symptoms can include blurred vision, paralysis, slurred speech, lack of coordination and incontinence. The severity of symptoms depends on how much damage has occurred.
MS is the most common disease of the central nervous system (the brain and spinal cord) affecting young adults in the UK. It currently affects around 85,000 people in the UK and can occur at any age, but in most cases symptoms first appear between the ages of 20 and 40. Women are almost twice as likely to develop MS as men. The majority of patients with MS have the relapsing-remitting form of the disease, characterised by attacks or relapses interspersed with periods of recovery or remission (Harbige and Sharief, 2007). It is a life-long condition, but it is not terminal and people with MS can expect to live as long as anyone else (NHS Direct, 2008c).
The cause of MS is not yet fully understood but is thought to be an autoimmune disease (like rheumatoid arthritis or type 1 diabetes) whereby the body’s immune system attacks its own tissues having ‘mistaken’ them for an invading (foreign) protein. This process is referred to as ‘molecular mimicry’ as part of the foreign protein closely resembles part of certain cells in our own body. If this all sounds a bit complicated, just think of it as ‘friendly fire’ – when a soldier mistakenly attacks one of his own. In autoimmune diseases, the body attacks itself.
As with other autoimmune diseases, it is thought that a combination of genetic factors and environmental factors causes the disease. There is undoubtedly an element of genetic predisposition in MS but the evidence suggests that this disease is more strongly related to environmental factors than genes. In other words, a person may have a genetic predisposition to the disease but not develop it unless exposed to a specific environmental ‘trigger’. Such triggers may include bacteria, viruses or components of the diet.
Geographical pattern
One of the most intriguing features of MS is that it occurs more in countries that are far from the equator. For example, MS is relatively common in the UK, North America and Scandinavia, but hardly ever occurs in countries such as Malaysia and Ecuador (NHS Direct, 2008c). The reason for this is not fully understood, but it could be that MS is triggered by a particular bacteria or virus which thrives in cooler climates. Alternative theories suggest that components of particular foods consumed in these countries may be responsible.
Diet and MS
Research suggests that some components in food can act as causative agents of autoimmune disease. For example, there is strong evidence that proteins found in cow’s milk can trigger an autoimmune response leading to type 1 diabetes in genetically susceptible children. The theory with MS is that proteins from certain foods (such as cow’s milk) may also prompt the immune system to respond inappropriately and attack the myelin sheath in the brain and central nervous system. A large body of evidence shows that populations that consume high quantities of animal-based foods seem to be most affected by MS (Agnello et al., 2004). This inevitably has drawn attention to the role of meat and dairy foods in the development of MS.
Numerous studies have revealed a striking association between the geographical pattern of MS and that of meat and dairy consumption (Arganoff and Goldberg, 1974; Butcher, 1976; Lauer, 1994). There is also strong evidence linking a high intake of saturated fat to the incidence of MS. Taken together, the evidence shows that foods rich in saturated fats are associated with higher levels of MS while foods rich in polyunsaturated fats are linked to lower levels (Harbige and Sharief, 2007).
The research investigating the links between diet and MS dates back 60 years to Dr Roy Swank’s work first at the Montreal Neurological Institute in Norway, then at the Division of Neurology at the University of Oregon Medical School in the US. Swank was intrigued by the geographical distribution of MS and hypothesised that dietary fat intake may contribute to progression of MS.
Swank suspected animal foods high in saturated fats may be responsible as MS seemed to occur most among inland dairy-consuming populations and less among coastal fish-eating populations. His best known trial, published in the Lancet in 1990, followed 144 MS patients for a total of 34 years (Swank and Dugan, 1990). Swank prescribed a low-saturated fat diet to patients with relapsing-remitting MS and observed how their conditions progressed. Results showed that those who adhered most closely to the diet derived the greatest benefits from the intervention. The beneficial effects were strongest in those who began to follow the diet early in their disease.
In 2000, 15 patients who had been on the diet for 50 years were re-assessed. Of these, 13 were able to walk without difficulty, the other two required assistance with walking (Swank and Goodwin, 2003). Swank concluded that if people with MS adhere to the diet, with no more than 10-15 grams of saturated fat per day, they can expect to survive and be ambulant and otherwise normal to an advanced age.
Although Swank’s diet restricted meat and dairy foods, it did include fish and fish oils. More recently, another study recommended a co-called ‘quasi’ vegan diet with fish oil (McCarty, 2001). This study concluded that a whole-food vegan diet, coupled with fish oil and vitamin D supplementation, may represent a practical strategy for the prevention of autoimmune diseases, while concurrently lowering the risk of many other life-threatening Western diseases. Both regimes overlook the fact that you can have an omega-3 rich vegan diet (containing ALA and an algal supplement containing DHA and EPA if desired) without exposing yourself to the toxins found in oily fish and fish oils.
Polyunsaturated fatty acids and MS
Some research indicates that polyunsaturated fatty acids (particularly omega-6 fats) have a role in the chain of events leading to, and the treatment of, MS. Studies show that omega-6 levels are lower in MS patients. It has been suggested that the way omega-6 fatty acids are normally processed in the body is disrupted in people with MS.
In a randomised, double-blind trial of a high dose and low dose omega-6 GLA-rich (borage) oil and a placebo control, the high dose had a marked clinical effect in relapsing-remitting MS. Results showed that the GLA-rich oil significantly decreased the relapse rate and the progression of disease (Harbige and Sharief, 2007). The authors of this study suggested that disturbed omega-6 fatty acid metabolism in MS gives rise to a loss of both long chain omega-6 fatty acids in the membranes and anti-inflammatory cytokines, particularly during the relapse phase.
The loss of these important neural fatty acids in central nervous system structure and function may have long-term consequences in MS. However, this feature of MS can be treated by supplementation (Harbige and Sharief, 2007). In general, it appears that over time, diets low in saturated fat, but containing both some omega-6 and omega-3 fats, can improve the course of MS (Harbige and Sharief, 2007).
In 2007, a Cochrane review concluded that polyunsaturated fatty acids seemed to have no major effect on the main clinical outcome in MS (disease progression) (Farinotti et al., 2007). However, only a limited number of studies was reviewed and they did state that the data available were insufficient to assess any potential benefit or harm from supplementation. Clearly more research is required to assess the effectiveness of dietary interventions in MS. In the meantime, over 50 per cent of people with MS make dietary changes and take supplements (Farinotti et al., 2007).
Polyunsaturated fats and autoimmunity
It is generally accepted that omega-6 fatty acids are pro-inflammatory (Harbige, 2003). However, while they have been shown to increase the severity of some autoimmune and inflammatory diseases, omega-6 fats may actually protect against other (immune-mediated and non-immune-mediated) inflammatory diseases. Therefore, the view that all omega-6 fats are pro-inflammatory is incorrect (Harbige, 2003).
There is some evidence that omega-3 fats can ‘dampen down’ inflammatory responses. This anti-inflammatory role may offer short-term benefits in some autoimmune diseases. However, this could be an undesirable long-term effect of high-dose fish oils, as it could compromise immunity (Harbige, 2003). As stated earlier, the inflammatory response is a natural part of our immune system and can help fight infection. In other words, a high intake of fish oils may not be beneficial in the long term; it may weaken the immune system while only addressing the secondary consequences of an autoimmune response.
Diets low in saturated fat and relatively high in omega-3 fats (higher than the low amount present in most UK diets) can reduce the severity of some autoimmune diseases. Conversely, diets high in the omega-6 fat LA may increase the severity of these conditions (Harbige, 2003). However, as stated previously, there is convincing evidence for a protective role of both omega-6 and omega-3 fats in MS (Harbige, 2003).
In conclusion, moderate intakes of omega-6 fats and the appropriate ratio between omega-6 and omega-3 fats are important for the correct functioning of the immune system (Harbige, 2003). Adjusting the ratio could be helpful in autoimmune or inflammatory disease. The optimum ratio varies depending on age and the basis of the autoimmune disease.
This all sounds rather complicated but the overall message is that a plant-based diet, low in fat, salt, sugar and processed foods and high in fresh fruit, vegetables, wholegrains, pulses, nuts and seeds can provide all the nutrients required for good health and reduce some of the risk factors for autoimmune diseases or prevent making an already existing condition worse.
As the incidence of most autoimmune diseases correlates directly to the consumption of animal foods, a move towards a more a plant-based diet could help combat the rise in these conditions among populations that currently consume high levels of dairy and meat products.
Allergies
Some research suggests that the dramatic increase in the consumption of omega-6 fats, coupled to the decrease in omega-3 fats consumed, is a major driver of the increase of a range of inflammatory allergic reactions (Chilton et al., 2008).
Asthma
Asthma is a chronic inflammatory lung disease characterised by recurrent breathing problems. The UK has one of the highest prevalence rates for asthma in the world, along with New Zealand, Australia and Ireland. Around one in eight children and one in 20 adults are currently being treated for asthma in the UK.
During an asthma attack, the lining of the airways becomes inflamed and the airways constrict. This can lead to the characteristic symptoms of asthma such as coughing, wheezing, difficulty in breathing and tightness across the chest.
The causes of asthma are thought to include a genetic predisposition (asthma in the family) and environmental triggers such as cigarette smoke, chemicals, dust mites and diet. As food allergies are responsible for approximately five per cent of all asthma cases (James et al., 1994) and as cow’s milk is a primary cause of food allergies, it seems reasonable to consider avoiding all cow’s milk and dairy products in the treatment of asthma.
Asthma may also respond to other dietary modifications, thereby reducing the need for medication. Studies show that supplementing the diet with plant-based fatty acids can inhibit inflammatory responses leading to asthma. One study found that supplementing the diet with omega-6 and omega-3 fats in a ratio of 2:1 helped alleviate symptoms, whereas a ratio of 10:1 made symptoms worse (Broughton et al., 1997).
Another study found that supplementing the diet with borage oil (containing GLA) led to the accumulation of natural inhibitors of leukotrines (hormones that cause the symptoms of asthma) within inflammatory cells (Chilton et al., 2008). This concurs with the research described above that shows that GLA provides an exception to the usual pro-inflammatory role attributed to omega-6 fats.
The overall optimum ratio of omega-6 to omega-3 fats may vary according the disease and the patient (age, sex and physical condition) but the message that we all need to increase our intake of omega-3 fats while not increasing that of omega-6 fats is consistent throughout the research.
Eczema
The increasing rate of eczema in the West has been linked to a steep rise in the consumption of omega-6 fats and the reduced intake of omega-3s (Koch et al., 2008). Omega-6 fats favour the formation of specific eicosanoids (hormone-like molecules) that are involved in allergic inflammation. The parent omega-6 fatty acid LA is converted into arachidonic acid, a precursor in the production of eicosanoids (Koch at al., 2008). Consequently an increased intake of omega-6 fats can promote allergic reactions, while increasing omega-3 intake competes with omega-6 metabolism and protects against inflammatory conditions.
The results of a recent exploratory trial were published in the British Journal of Dermatology (Koch at al., 2008). This study reported how 53 patients suffering from eczema were randomly allocated supplements of both DHA and EPA, or a control (caprylic acid, otherwise known as octanoic acid, an eight-carbon saturated fatty acid) daily for eight weeks. Results showed a considerable improvement in the group taking DHA/EPA supplements. The authors suggested that these fatty acids may have an anti-inflammatory role as they inhibit arachidonic acid production. While some arachidonic acid is essential for your health, too much may make inflammation worse.
It was noted that plasma DHA and EPA levels rose two- to threefold following supplementation. The authors suggested that the higher level of EPA might have resulted from the small but significant amount of EPA in the supplement or from the retroconversion of DHA to EPA. This is important as it indicates that an algal supplement supplying DHA could be used to increase both DHA and EPA levels. Again this means you could take an algal supplement and avoid the risk of exposing yourself to toxins that may be found in fish oil supplements.
Summary
Our genes take a very long time to change and are still very similar to the genes of our ancestors during the Palaeolithic era 40,000 years ago, when the human genetic profile was established (Simopoulos, 2008). The same cannot be said for our diet. Anyone can see our diets have changes hugely – our ancestors would have been hard pushed to find burger, chips and a milkshake! But does this matter? Well, studies on the evolutionary aspects of diet indicate that the major changes that have occurred have altered the type and amount of essential fatty acids in our diets (Simopoulos, 2008). So while in many ways our bodies are potentially the same as those of our ancestors, the way we fuel it has changed drastically. This is like expecting a car to run on a lower grade fuel than it was designed for. There will inevitably be problems with the engine.
The increase in heart disease, arthritis, allergies and other health problems has encouraged some scientists to investigate the role of diet in these and other diseases. Omega-3 fats have been identified as potentially helpful. Many people cannot tolerate the taste or smell of fish oils, even when provided in capsules. Because of this, and dwindling fish stocks, interest in plant-based sources of omega-3 fatty acids has increased tremendously (Chilton et al., 2008).
Most fat eaten in excess of requirements is stored in adipose tissue in the form of triglycerides (three fatty acids combined with glycerol). Many diseases feature elevated levels of triglycerides: cardiovascular diseases, asthma, diabetes, obesity and arthritis. There is tremendous interest in plant-based oils and supplements (as an alternative to fish oil) as a source of omega-3 fatty acids for protection against these chronic diseases. Researchers from the Center for Botanical Lipids at Wake Forest University in North Carolina state that botanical (plant-based) oils hold particular promise for modulating inflammatory responses (Chilton et al., 2008).
A large number of vegetarian and vegan studies show that plant-based diets offer numerous health benefits, including the prevention and therapy of many chronic diseases including arthritis (Leitzmann, 2005). Since vegetarian and vegan diets are more sustainable, environmentally and economically, they certainly deserve more consideration in both the prevention and treatment of disease. This message needs to filter down from the peer-reviewed studies into our hospitals, schools, workplaces and homes.
Brain food
The human brain grows and develops very rapidly during the first year of life, tripling in size by the age of one. The brain is largely made up of fat (over 60 per cent) and early brain development and function in humans requires a sufficient supply of polyunsaturated EFAs. For humans, the omega-6 fat arachidonic acid and the omega-3 fat DHA are essential for brain development and functioning.
Although human breast milk and cow’s milk contain a similar amount of total fat, the proportion of saturated and unsaturated fats in each is very different. This difference contributes to the unsuitability of cow’s milk for human infants. The high level of unsaturated fats in human breast milk reflects the crucial role these fats play in human brain development. A rapid increase in body size is more important for cows, so they produce milk high in body-building saturated fats to help their calves grow quickly.
A review of 20 studies of cognitive (brain) function of breast-fed infants compared to that of formula-fed infants concluded that the nutrients in breast milk may have a significant effect on neurological development in infants (Anderson et al., 1999). Indeed, a longer duration of breastfeeding is associated with significantly higher scores in verbal, performance and IQ tests (Mortensen et al., 2002). So breast really is best!
Attempts to alter the fatty acid composition of cow’s milk, in order to meet human requirements, have involved experiments feeding cows fish meal and soya beans (Abu-Ghazaleh et al., 2004) and flaxseed (Petit, 2002). Feeding flaxseed resulted in a lower omega-6 to omega-3 fatty acid ratio, which might improve the nutritional value of milk for humans. Of course you could just eat flaxseed oil yourself to improve the balance of omega-3 and omega-6 oils in your diet while avoiding the many undesirable components of cow’s milk and oily fish.
Smart enough to be veggie?
Fish oils have been sold as a magic bullet for boosting brain power. As the term ‘essential’ implies, we certainly do need some EFAs in the diet. However, contrary to the intensive and misleading marketing, fish and fish oils are not essential for good health. In fact, the fatty acids found in fish oil (EPA and DHA) are not defined as ‘essential’; only the plant-based fats ALA and LA are. These plant-derived EFAs provide a healthier and safer source. Consider this: if fish oils were a superior source of fatty acids for brain health then vegetarians would come bottom of the intelligence stakes. The reverse appears to be the case.
Links between intelligence and the vegetarian diet were demonstrated in 2006 when a team of vegetarians won the BBC’s Test the Nation IQ battle (the butchers came joint fourth; sadly there was not a team of fish-mongers!)
More weighty evidence was provided in a study published in the British Medical Journal which showed that intelligent children are more likely to become vegetarians later in life (Gale et al., 2007). Researchers from Southampton University found that people who are vegetarians by the age of 30 had an IQ five points higher than the average IQ when they were 10. This might explain why people with a higher IQ are healthier: vegetarians generally suffer less heart disease, hypertension, obesity, diabetes, various cancers, diverticular disease, bowel disorders, gallstones, kidney stones, and osteoporosis.
The obvious point here is that if omitting fish and fish oils from the diet led to a lower cognitive ability, non-fish eating children and adults would come bottom in the intelligence stakes. There has never been any study to suggest this is the case and thousands of healthy intelligent vegetarian and non-fish eating families provide proof that brains function perfectly well without fish oils!
Fish oils for brainy kids?
So what is the scientific evidence that fish oils can improve cognitive ability and where does the Government stand on this issue? The evidence comes mainly from trials done using children with behavioural problems and is largely anecdotal.
The Durham-Oxford Study is the most cited work (Richardson and Montgomery, 2005). In this study, 117 children with developmental coordination disorders (DCD) such as attention deficit/hyperactivity disorder (ADHD), dyslexia and dyspraxia were given a daily supplement of fatty acids. The treatment was a supplement containing 80 per cent fish oil and 20 per cent evening primrose oil in gelatine capsules. The daily dose of six capsules provided omega-3 fatty acids (558 mg of EPA and 174 mg of DHA) and the omega-6 fatty acid LA (60 mg), or olive oil (omega-9) as a placebo.
After three months of treatment, results showed significant improvements in reading, spelling and behaviour among those receiving the fish oil supplements. The researchers concluded that fatty acid supplements may be a safe, tolerable, effective treatment for improving academic progress and behaviour among children with DCD. In other words, children who are not fulfilling their potential may benefit from increasing their intake of essential fatty acids. The VVF asked the researchers in Durham if they would consider using flaxseed oil in future trials to see if similar results could be achieved without exposing children to potential toxins but our requests were ignored.
A follow-up trial was conducted in Durham more recently whereby three million fish oil capsules were given to 2,000 children over eight months to see if their GCSE results improved. Unfortunately the GCSE results were rather disappointing, which was not press-released by the County Council. In some very fast back-pedalling they said “…it was never intended, and the County Council never suggested, that it would use this initiative to draw conclusions about the effectiveness or otherwise of using fish oil to boost exam results.” So it seems fish oil was not the magic bullet Durham Council was looking for.
It is interesting to note that the fish oil capsules used in the Durham trial cost 80p per child, per day, rather more than the 65p Durham Council was spending per child per day on school meals at the time. In 2008 the cost of ingredients had risen, but to just 80p for a secondary school child per day (Durham Council, 2008). Rather than looking for a magic bullet, improving the quality of school meals and education about diet and health would perhaps have been a better approach.
Most children in the UK eat such appalling diets that nutritional deficiencies are inevitable. Correcting such deficiencies will in many cases improve the symptoms associated with that particular deficiency. This is not the same as saying fish oil will turn all kids into geniuses, which is exactly how the media interpreted the findings. ‘Council to include more fruit, vegetable and wholefoods in school meals‘ just doesn’t make such an impressive headline as ‘magic pill makes kids clever‘.
The Joint Health Claims Initiative (JHCI) operated between 2000 and 2007 to ensure a level playing field for the food industry and to increase consumer protection by investigating the science behind health claims (JHCI, 2007). It is no longer in operation as the new EU ‘claims’ regulation for foods now verifies health claims. However, during the seven years of investigating health claims, the JHCI approved claims for soya protein, oats and reduced saturated fat all for their cholesterol-lowering effects and for wholegrain foods’ benefits to heart health. They also approved health claims for long chain omega-3 fats for maintaining a healthy heart. They did not approve any claims linking omega-3 fats (or fish oils) to cognitive ability.
Unfortunately misleading publicity from this and other research has encouraged companies to produce so-called functional foods such as St Ivel Advance Omega-3 milk. The advertisements implied that this milk may make children more intelligent because it contained omega-3 fatty acids (from fish). The advertisements for this so-called ‘clever milk’ featured the scientist Professor Robert Winston, lending kudos to the outlandish claims. But following complaints, the Advertising Standards Authority (ASA) ruled that the advertisements were misleading and the claims used for the benefits of the milk unproven. The ASA ruled that as the children in the trial had learning difficulties, there was no basis to claim there would be an improvement in the concentration of all children. Dairy Crest, the firm behind the product, withdrew the adverts following the ruling.
Although the Government has refused to shift its position on recommending fish oils for heart health, it is clearly not convinced about cognitive benefits. The FSA states that: “Evidence on the cognitive benefits of the omega-3 fatty acids, EPA and DHA, which are found in fish oils, is currently uncertain,” (FSA, 2008).
Common sense suggests that if the diet provides enough EFAs, fish oils may have no additional effect on cognitive ability at all. Encouraging children to eat oily fish in the pursuit of cleverness may lead to serious health problems due to their exposure to pollutants.
All of the world’s oceans and rivers are polluted with toxic chemicals; mainly pollutants resulting from decades of increasing industrial activity. The health risks associated with the consumption of fish and fish oil supplements are due to the presence of these toxic pollutants, not to mention the saturated fat, animal protein and cholesterol they contain. Oily fish such as salmon, trout and mackerel may be contaminated with chemicals, while shark, marlin and swordfish contain high levels of mercury (Consumers’ Association, 2002). Long-term exposure to these harmful substances poses a significant threat to health.
POP goes the seawall:
A particularly nasty class of contaminants found in oily fish is known as persistent organic pollutants (POPs). These organic pollutants are made up of complex molecules which do not break down easily in the environment; hence the name ‘persistent’. They build up in the food chain through bioaccumulation. This means that the level of chemicals found in an animal tissue rises the higher up the food chain the animal is. For example, larvae might eat some contaminated algae, a fish then eats the larvae, and a bigger fish eats smaller fish and so on. Fish at the top of the food chain such as tuna, shark, swordfish, tilefish and king mackerel, have the highest concentrations of POPs. Algae (which are right at the bottom of the food chain) are likely to contain much lower levels.
Farmed salmon are even more of a concern than wild salmon due to the concentration of POPs in the feed they eat and their fatty nature as POPs can accumulate in fatty tissue.
In 2001, officials from 90 countries signed a landmark UN treaty in Stockholm, designed to curb the use of some of the world’s most dangerous and toxic chemicals (Stockholm Convention, 2008). They identified twelve particular substances for banning which later became known as the ‘dirty dozen’. The list included eight organo-chlorine pesticides: aldrin, chlordane, DDT, dieldrin, endrin, heptachlor, mirex and toxaphene; two industrial chemicals: hexachlorobenzene (HCB) and polychlorinated biphenyls (PCBs); and two groups of industrial by-products: dioxins and furans.
The Stockholm Convention on POPs came into force on May 17, 2004, with agreement from an initial 128 parties and 151 signatories. Co-signatories agreed to ban nine of the ‘dirty dozen,’ limit the use of DDT to malaria control and curtail production of dioxins and furans. Several other substances are now being considered for inclusion in the Convention. These are: hexabromobiphenyl, octaBDE, pentaBDE, pentachlorobenzene, short-chained chlorinated paraffins, lindane, a- and ß-hexachlorocyclohexane, dicofol, endosulfan, chlordecone and PFOS. Not what you’d expect to see in a list of ingredients!
However, even though this is a step in the right direction, it will take many years for POPs (used in everyday items such as plastics, paints and pesticides) to break down. Furthermore, the environmental group, the World Wildlife Fund has expressed concerns that global warming could increase levels of POPs as higher temperatures may release chemicals which have been frozen in glaciers.
PCBs:
Polychlorinated biphenyls (PCBs) and dioxins are the main contaminants in oily fish (Consumers’ Association, 2002). Although they are now banned, PCBs have not disappeared from the environment and won’t for a very long time.
The Scientific Advisory Committee on Nutrition (SACN) is an advisory committee of independent experts that provides advice to the FSA, Department of Health and other government agencies and departments. SACN states that: “PCBs are very persistent chemicals which are ubiquitous in the environment and are generally present in low concentrations in foods, especially fat-containing foods including milk, meat and fish,” (SACN, 2004).
As persistent lipophilic (fat-loving) compounds that accumulate in lipids, PCBs are particularly likely to be present in oily fish. They are implicated in heart disease, cancer, infertility and can harm developing foetuses by disrupting the development of male babies’ reproductive organs.
Dioxins:
Dioxins were the primary ingredient in Agent Orange, the defoliant sprayed over Vietnam which has produced an appalling legacy of cancers and other diseases, miscarriages and birth defects. As stated, these insidious toxins build up in the body over time. The FSA points out that: “If a woman changes her diet when she becomes pregnant, or when she starts trying for a baby, this won’t change the levels of dioxins and PCBs that are already in her body. So it’s a good idea to limit the amount of oily fish eaten from a young age.”
Furthermore, contrary to previous advice that these toxic pollutants are only found in oily fish, the FSA states that: “Recent surveys have shown that some other fish and crab may also have similar levels of dioxins and PCBs as oily fish. These fish are: sea bream, turbot, halibut, dog fish or huss, and sea bass.” Now they tell us!
Mercury rising:
Methylmercury is the organic form of mercury found in the environment, usually as the result of industrial pollution. This toxin is commonly found in the marine environment and accumulates up the food chain particularly in older, larger fish. Mercury affects the kidneys, heart and central nervous system (CNS). Exposure is particularly hazardous for unborn children where the main organs and the CNS are still developing. Women and girls who may have children one day are advised to eat less oily fish than men and older women because mercury can harm the development of unborn children. The FSA states that adults should have no more than one portion of swordfish, shark or marlin a week because these fish contain high levels of mercury (FSA, 2009).
While some studies indicate that high intakes of oily fish, or fish oil supplements, are associated with a reduced risk of CVD, others have suggested that fish oils can increase the risk. In these studies, mercury is suspected as being responsible for the harmful effects seen as it can accelerate atherosclerosis and increase the risk of heart attack. Possible mechanisms by which mercury exerts these damaging effects include promoting the peroxidation of unsaturated fatty acids (Salonen et al., 1995). This is the process whereby damaging molecules called free radicals ‘steal’ electrons from the fats in cell membranes, resulting in cell damage.
Mercury also forms an insoluble complex with the antioxidant mineral selenium. It binds it in an inactive form preventing selenium from acting as a cofactor for the protective enzyme glutathione peroxidase. This enzyme’s main biological role is to protect the body from oxidative damage. Binding selenium in this way can lead to an increase in free radical activity. Mercury also has a very high affinity to sulfhydryl groups which play an important role in antioxidant reactions. Sulfhydryl groups are compounds that contain a functional group composed of a sulphur atom and a hydrogen atom (-SH). They feature as a functional group of the amino acid cysteine and so play an important role in many biological systems. By binding to sulfhydryl groups, mercury inactivates antioxidative compounds, again, increasing free radical activity. Taken together, these reactions indicate how mercury could inhibit important antioxidative mechanisms in humans. In other words, the high mercury content in fish can not only counteract the protective effects of the fatty acids found in oily fish, but may go on and do serious harm to health.
For non-oily fish, there seems even less reason to take the risk of exposing yourself to mercury. Numerous studies have reported an association between fish intake and coronary mortality. In 1995, one study investigated why men in Eastern Finland have an exceptionally high level of mortality from CVD (Salonen et al., 1995). This study measured hair mercury content in healthy individuals and then recorded CVD events (such as heart attacks) over the following years.
The mercury content in Finnish lakes is known to be relatively high; especially so in ground waters (water that supplies wells and springs) in Eastern Finland. This study found that an average daily fish intake of just 30 grams or more was associated with a two-fold increase in heart attack risk. For each additional 10 grams of fish per day there was an increment of five per cent in the five-year risk of heart attack. This indicates that mercury, even in subtoxic amounts, is a risk factor for coronary and fatal CVD. The authors concluded that because in many countries fish and seafood are contaminated with mercury and because fish is eaten all over the world, their findings could be of enormous public health importance.
A later study (from the same group) investigating the association between blood levels of the omega-3 fats EPA and DHA, and the risk of acute coronary events in middle-aged men from Eastern Finland, again looked at mercury levels in hair (Rissanen et al., 2000). This prospective population-based study of 1,871 men confirmed that high levels of DHA in the blood were associated with a decreased risk of acute coronary events. However, the men who fared best in this comparison were those with high DHA levels and low mercury content in the hair. It was concluded again that mercury could cancel out any protective effect offered by the fats in oily fish.
A case-controlled study published in the New England Journal of Medicine in 2002 conducted in eight European countries and Israel provided further evidence linking mercury in fish to CVD. This study investigated the relationship between mercury levels in toenail clippings and DHA levels in adipose tissue with the risk of a first heart attack among men (Guallar et al., 2002). This study included 684 men in the coronary care units of participating hospitals who had experienced their first heart attack. Also, 724 men representative of the same population (but who had not had a heart attack) were selected to act as controls. Results showed that while higher DHA levels were associated with a lower heart attack risk, the toenail mercury level was directly associated with an increased risk of heart attack. The authors concluded that mercury may diminish the cardioprotective effect of fish intake.
They also warned that exposure to mercury is already a concern in specific high risk groups and suggested extending the US Food and Drug Administration’s recommendation that pregnant women and women who may become pregnant do not eat swordfish, king mackerel, tilefish or tuna to include the entire population.
A statement from the American Heart Association (AHA) acknowledges the discrepancy in the findings of research on fish oils and CVD (Kris-Etherton et al., 2002). They acknowledge that the contradictory findings of these studies could be explained by the adverse effects of mercury, which they say may diminish the health benefits of omega-3 fatty acids from fish. They conclude that while collectively, the research is supportive of the recommendation to include at least two weekly servings of fish (particularly fatty fish), this recommendation must be balanced with concerns about environmental pollutants, in particular PCB and methylmercury. This ambiguity can only add to the confusion!
They do however point out that the research supports the inclusion of vegetable oils (soya bean, rapeseed, walnut and flaxseed oils) and food sources (walnuts and flaxseeds) high in ALA in a healthy diet for the general population. This, at least, is a move in the right direction.
Food Poisoning:
Food poisoning generally happens when someone eats food that is contaminated with bacteria or its toxins. According to the FSA, it is estimated that up to 5.5 million people in the UK are affected by food poisoning each year (NHS Direct, 2008d). However, it is difficult to know exactly how many people are affected as not all of those affected seek medical advice.
Most cases of food poisoning result from eating contaminated animal products (meat, poultry, eggs, dairy, fish and shellfish) as plants tend not to harbour the types of bacteria capable of causing food poisoning in humans. If plant foods do cause food poisoning it is generally because they have been contaminated with animal excreta, human sewerage or prepared with dirty hands.
While most food poisoning incidents are associated with meat and poultry, the links between fish, shellfish and food poisoning should not be discounted. Researchers from the Health Protection Agency Centre for infections in London looked at a number of cases of food poisoning in the UK between 1992 and 2003 (O’Brien et al., 2006). Of the 1,763 cases reported to national surveillance, only 55 were published in the peer-reviewed literature. As this type of publication tends to favour the unusual or novel event, coverage can lead to an over-emphasis of one food group over another. This has lead to a failure to pay enough attention to the role of contaminated fish and shellfish in food poisoning. The authors of this study suggest that relying solely on the literature has lead to an over-emphasis on controlling the milk supply and a failure to pay enough attention to the role of contaminated fish and shellfish in food poisoning.
When they are raw or haven’t been cooked properly, fish and shellfish can contain a range of harmful viruses and bacteria. Shellfish (such as clams, mussels and oysters) are also filter feeders, constantly filtering water, which can lead to the accumulation of pollutants. The FSA recommends that elderly people and people who are unwell might want to avoid eating raw shellfish to reduce their risk of food poisoning (FSA, 2008d). Most shellfish is eaten cooked, but oysters are often served raw and can contain a virus called the Norovirus. Raw or partially cooked shellfish can also contain hepatitis A, which is a highly contagious virus of the liver.
For these reasons, the VVF argues that sea vegetables (seaweed) are the true ‘fruits de mer’ or fruits of the sea, not shellfish. Not only do they add flavour to food, each variety is a low-fat nutritional powerhouse, packed full of vitamins and minerals. Plus, you won’t find elevated levels of dioxins, PCBs or mercury in sea vegetables, in contrast with fish and shellfish in whose body fats these pollutants accumulate over time.
The FSA’s website provides an extensive list of precautionary measures people should take when buying, storing and preparing fish. It lists 18 different ways you can minimise the risk of being poisoned (FSA, 2009). Of course just avoiding fish and shellfish would be much easier. Indeed excluding all animal foods from the diet will dramatically decrease the risk of food poisoning.
Fish and PhIPs:
Most people think the fool-proof way to avoid food poisoning from meat and fish is to cook it very well – some people practically cremate it to make sure. However, thoroughly cooking meat and fish can lead to even more serious problems.
Cancer-causing compounds called heterocyclic amines (HCAs) are formed when meats (such as beef, chicken and pork) and fish are cooked at high temperatures (Wilson et al., 2007). HCAs form when a chemical found in muscles called creatine reacts with amino acids (the building blocks of protein) and sugar at high temperatures. While meat and fish contain significant amounts of creatine, vegetables contain none.
In 2005, the US federal government officially added HCAs to its list of known carcinogens (US Department of Health and Human Services, 2008). The most abundant HCA found in the human diet is called 2-amino-1-methyl-6-phenylimidazo[4,5-b] pyridine (PhIP). PhIP is associated with an increased risk of cancer of the colon, breast and prostate (Wilson et al., 2007).
Exactly how PhIP increases cancer risk is uncertain. It has been suggested that PhIP produces harmful molecules called reactive oxygen species which cause DNA strands to break thus increasing cancer risk (Wilson et al., 2007). Alternatively, researchers at Imperial College in London have reported that PhIP is a potent mimic of the hormone oestrogen (Lauber et al., 2007). This is very worrying, as many studies link higher oestrogen levels to breast cancer. This theory provides a plausible explanation for why diets rich in red meats are linked to an increased risk of breast cancer.
In 2005, the Physician’s Committee for Responsible Medicine’s Cancer Project revealed that grilled salmon was among the five worst foods to grill (PCRM, 2005). The Cancer Project nutritionists found that many commonly grilled foods contain alarmingly high levels of HCAs. The five foods containing the highest levels included: chicken breasts, steak, pork, salmon and hamburgers.
The amount of PhIP in some foods may typically lie in the region of 35 nanograms per gram. However, there are some reports of much higher levels of PhIP (Skog, 2002). Concentrations of PhIP in fish vary widely according to the type of fish and method of cooking. One study reported levels ranging from 1.7 to 73 nanograms per gram in salmon cooked at 200°C by various methods (Gross and Grüter, 1992).
The damaging action of HCAs may be reduced by foods containing antioxidants, such as vegetables and soya foods (Weisburger, 2002). However, the safest option is to avoid meat and fish altogether. Healthier options for grilling and frying include soya burgers, veggie sausages and Portabella mushrooms.
Unless you seek out wild fish, the chances are that most of the fish you see in shops and restaurants were raised on a fish farm in an environment very different to what their wild counterparts would have experienced. One of the main differences on many fish farms is the stocking density – imagine having to fight your way through the January sales every day just to get something to eat. This is the type of scenario many farmed fish endure.
Fish species raised by fish farms include salmon, catfish, tilapia, cod, carp, trout and others. Just as we see with other farmed animals such as the dairy cow, intensive farming methods results in a cheaper end product (in terms of quality and price). This is why farmed salmon has been called ‘the battery chicken of the seas’. This may not concern you if the supposed health benefits are the same. However, they are not.
From a nutritional and health perspective, there are several important differences between farmed and wild fish. In the wild, salmon can eat 10 times their own body weight per day. Providing a similar diet to farmed fish would mean grinding up to 10 pounds of sardines, anchovies, mackerel, herring and other fish for every pound of pale and sickly farmed salmon produced. This is clearly uneconomical for fish farmers and heralds an ecological disaster as one-third of the global fish catch ends up as fishmeal or fish oil and fish farms use about half of the fishmeal and more than 80 per cent of the fish oil (Soil Association, 2008).
It is much cheaper to manufacture feed pellets from soya, rapeseed or corn with animal by-products and vitamin and mineral supplements. In Canada and Chile, it is common to use other protein sources such as feather or blood meal by-products of chicken and pig production (Soil Association, 2008a). Consequently, farmed fish tend to contain more total fat, but less omega-3s than their wild counterparts (Weaver et al., 2008). In other words, the levels of good and bad fats (the fatty acid profile) of farmed fish vary widely from that of wild fish.
Using cheaper vegetable-based feeds drives up the level of omega-6 fats found in the fish. Farmed tilapia (the most rapidly expanding fish in terms of world and US consumption), contain some of the highest levels of the omega-6 fatty acid arachidonic acid found in our food chain (Weaver et al., 2008). These and other farmed fish have a fatty acid profile that would generally be considered as unhealthy. Indeed, marked changes in the fishing industry during the past decade have produced widely eaten fish that have fatty acid characteristics that are generally accepted to be inflammatory by the health care community (Weaver et al., 2008).
The fish used in organic fish feeds come from the discarded filleting wastes (blood, guts, tails and heads) of fish caught for human consumption and should not contain fish caught specifically for fish feed. However, this does mean the supply is sustainable; human demand for fish also exceeds supply. Compared to conventional fish feed, organic fish feed may use more fish-based ingredients than non-organic fish feed but still might only have 40 per cent fishmeal and about 22-25 per cent fish oil (Soil Association, 2008a). This means that 35 per cent of the feed could be vegetable-based.
Farmed fish can also contain chemical pesticide residues as well as dangerous levels of toxic man-made chemicals including PCBs. A 2002 study investigating the levels of toxins in commercial salmon feeds, farmed salmon and wild salmon found that the farmed salmon had consistently higher levels of a range of contaminants including PCBs (Easton et al., 2002). The authors suggested that the higher levels seen in the farmed salmon probably resulted from the elevated level of contamination found in the commercial salmon feed. They concluded that this analysis indicates a safety concern for individuals who, on a regular weekly basis, consume farmed salmon produced from contaminated feed. Since then, other studies have indicated that commercial feed is likely to be a major source of PCBs in farmed salmon (Carlson et al., 2005).
So, farmed fish are very far from the safe choice we are led to believe and from a health perspective, when fish are farmed, they lose some of their protective fats. This is a ridiculous situation where the one possible argument in favour of fish consumption (their omega-3 content) is being eroded by intensive farming methods. There remains little, if any, argument for consuming fish.
Fish oil supplements
Some people prefer to take fish oil supplements rather than eat oily fish. However, fish oil supplements have also been linked to negative health effects in numerous studies. This is particularly worrying as they are increasingly popular as clever marketing persuades people to buy them.
Most fish oil supplement manufacturers publicise their meticulous manufacturing techniques reassuring us that all toxins are removed from their products. However, in March 2006, the FSA announced that the fish oil supplement manufacturer Seven Seas Ltd withdrew a number of batches of its own fish oil supplements because the levels of pollutants present (FSA, 2006). Less than a month later Boots withdrew fish oil capsules for the same reason (FSA, 2006a). In both cases they said although there was no health risk associated with consumption of this product, the level of dioxins found in fish oil used to produce these capsules exceeded statutory limits. This is a bizarre statement which seems to be saying that a little bit of poison should be all right!
The official position – not budging
The seriousness of the potential health risks of consuming toxins in fish prompted a joint subgroup of two advisory committees, the Scientific Advisory Committee on Nutrition (SACN) and the Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment (COT), to consider the benefits and risks of fish consumption (SACN, 2004).
Their report formed the basis of the FSA advice that pregnant and breastfeeding women should limit their consumption of oily fish to one to two 140 gram portions per week. This group (and children under 16) they say, should avoid shark, marlin and swordfish and not eat large amounts of tuna because of the potential methylmercury exposure. Men, boys and women past childbearing age or who are not intending to have children can eat up to four portions of oily fish a week before the possible risks might start to outweigh the benefits.
The report highlights the presence of dioxins in herring, salmon, mackerel and to a lesser degree in trout, and voices concerns about the presence of other pollutants such as brominated flame retardants. The FSA states that occasionally eating more than the recommended amounts of oily fish will not be harmful. It says that the risks from chemicals such as dioxins are not immediate; they develop as the chemicals accumulate in the body over a long period of time. Surely it is better to avoid these hazardous chemicals altogether?
Confused? You will be!
The FSA advises that fish oils protect against CVD and that long chain omega-3s are vital for the development of the central nervous system of the foetus and the breast-feeding infant (SACN, 2004). However, the FSA warns pregnant and breast-feeding women to restrict their intake of oily fish to limit their exposure to harmful toxins. So just when your intake of omega-3 really matters, during pregnancy and when you are breastfeeding, the Government warns you to limit your intake! Consumers are unsurprisingly confused; the information given is neither comprehensive nor consistent.
In 2002, Which? magazine reported the findings of a Consumers’ Association survey which asked 972 adults about their awareness of, eating habits and attitudes to oily fish (Consumers’ Association, 2002). The survey found that only a sixth of fish-eaters knew that the FSA’s advice is to eat oily fish once a week; over half thought the advice was to eat two or more portions. A shocking 61 per cent of people had no idea that oily fish may contain contaminants. One per cent knew that pregnant women should avoid certain fish but nobody could name them. Most people in the survey were confused by what was meant by oily fish (14 per cent thought that cod was an oily fish). It is not just the public who are confused; the Consumers’ Association states that the FSA couldn’t provide any clear answers about the health implications of eating more than one portion of oily fish per week.
It’s no clearer in the US. In 2002 the American Heart Association (AHA) issued a statement supporting the recommendation for at least two servings of fish (particularly oily fish) per week (Kris-Etherton et al., 2002). However, the AHA warned that the recommendations on fish consumption need to be balanced with concerns over contamination of fish with environmental pollutants (particularly mercury and PCBs). This is an incredibly important proviso which seriously challenges the idea that fish is ‘healthy’. It should be noted that the AHA also recommended plant foods that are high in the plant omega-3 ALA such as soya beans, rapeseed, walnuts and flaxseed and oils made from them.
In the joint WHO/FAO 2003 report Diet, Nutrition and the Prevention of Chronic Diseases, regular fish consumption of one to two servings per week is recommended to protect against CVD (WHO/FAO, 2003). However, whilst it also states that vegetarians can ensure adequate intakes of the omega-3 fatty acid ALA from plant sources, the report fails to give any warnings about the dangers of environmental contamination.
This conflicting advice has led to much confusion. Who should the public listen to? Who can they believe?
Fish is not a popular food
Despite the constant barrage of fish-promoting marketing and hype, the UK public just don’t buy it! The FSA says that on average, people in the UK eat only a third of a portion of oily fish a week (FSA, 2004). Indeed, fish is so unpopular that the FSA admits that seven out of 10 people in the UK don’t eat any oily fish at all. Clearly then, oily fish is not a significant contributor of omega-3 fatty acids in the diets of many people.
From a public health perspective, encouraging people to eat more fish in order to gain healthy amounts of omega-3 fats is simply not working. Even if people did start to consume more, the oceans simply cannot cope with any more demand, and as we have seen, farmed fish is definitely not the solution.
The upshot of all this confusion and dislike for fish is that many people fail to understand the importance of omega-3s and do not realise how easy it is to obtain them from every-day plant foods. Promoting oily fish as the only ‘heart friendly’ solution could actually deter individuals from making the fundamental dietary changes necessary for real long-term heart and body health. A healthier and simpler solution would be to promote a plant-based diet containing EFA-rich seeds, nuts and oils. Plants, not fish, are the way forward for good health.
Plant EFAs leading the way to good health
The good news is you don’t have to eat neurotoxins and carcinogens to get your omega-3 fatty acids; there are perfectly safe plant sources that can benefit your health.
Antioxidants in plants protect EFAs
The antioxidant vitamins C, E and beta-carotene (the precursor of vitamin A) are found in abundance in plant foods such as fresh fruits, vegetables, nuts and seeds. They are thought to be one of the body’s main defences against damaging molecules called free radicals. They are also vital for another important function that demonstrates why plant sources of fatty acids are superior to fish-derived versions.
Most people (especially those who cook a lot) know that certain fats are more likely to ‘go off’ when they are exposed to air. The difference arises from the number of double bonds in the fat as they make fats vulnerable to attack from oxygen molecules. This is why we cover food with plastic wrap or submerge it in water to protect it. This is why fish oils are prone to oxidation and give off a characteristic ‘fishy’ smell.
Antioxidants help slow this decaying process by acting as a fall guy for the fatty acid; they take the oxygen hit and save the fat from oxidative damage. Plant sources of EFAs, such as nuts and seeds, possess their own supply of antioxidants which protect their fats (in particular vitamin E). So yet again, we see why a plant-based diet provides not only important nutrients, but valuable substances that can protect us from oxidative damage too.
Free radicals are a problem for us too! They are unstable molecules generated by normal bodily functions, cigarette smoke, pollution, ultraviolet light and stress. Free radicals are linked to cancer or other diseases as well as the aging process. Animals and plants protect themselves against free radicals with antioxidants. They are a natural self-defence mechanism which is thought to defend against many diseases in humans, including the UK’s biggest killers heart disease and cancer.
As stated, the three amigos of the antioxidant world are beta-carotene (vitamin A), vitamin C and vitamin E. The mineral selenium is another valuable antioxidant. Antioxidants are not found abundantly in meat or fish. Plant foods (including fruit, vegetables, nuts and seeds) are the best sources. In the largest, most comprehensive analysis to date of the antioxidant content of commonly consumed foods cranberries, blueberries and blackberries ranked highest among the fruits studied. Beans, artichokes and Russet potatoes topped the list of vegetables. Pecans, walnuts and hazelnuts were the top nuts and ground cloves, cinnamon and oregano ranked highest among the herbs and spices (Wu et al., 2004). As a general rule, brightly coloured vegetables (such as sweet potatoes, red cabbage and tomatoes) tend to be relatively high in antioxidants.
Again, vegans are in a win-win situation. Not only do they avoid harmful substances found in meat and fish, they also benefit from a wide range of healthy nutrients including fibre, vitamins, minerals and of course, antioxidants.
Sustainability
The widely publicised supposed health benefits of omega-3 fats from fish, together with dwindling supplies of fish caught from the wild, have spawned a dramatic expansion in aquaculture (farmed fish). Aquaculture has increased at an annual rate of 9.2 per cent compared with 1.4 per cent for caught fish (Weaver et al., 2008).
Nearly half the fish consumed as food worldwide (43 per cent) is raised on fish farms rather than caught in the wild; that’s up from just nine per cent in 1980 (FAO, 2006). The level of fish caught in the wild (around 90-93 million tonnes annually) by contrast, has not changed much despite growing world population and demand. It can’t. The FAO acknowledges that there is little chance of any significant increase in catches beyond these levels anyway.
The levelling off of wild catches coupled with the growing world population and increasing demand for fish spells trouble says the FAO. It estimates that an additional 40 million tonnes of aquatic food will be required by 2030 just to maintain current levels of consumption. This is clearly unsustainable, we have to look to alternatives, and fish farming is not the answer. The environmental problems such as the spread of disease, sea lice and pollution associated with farmed fish are abundant. The sensible, and in fact the only answer is to obtain our omega-3 fats from sustainable plant sources.
Recommendations
A well-balanced plant-based diet containing green leafy vegetables, wholegrain foods, pulses, nuts and seeds will ensure an adequate intake of the plant omega-3 ALA. One of the best sources is flaxseed oil, containing 57 per cent ALA and 16 per cent LA with a omega-6:omega-3 ratio of 0.28:1 (Davis and Kris-Etherton, 2003). A 14 gram tablespoonful of flaxseed oil provides eight grams of ALA. Flaxseed oil must be kept in the fridge and added to sauces and dips or cooked food. Cooking with it will destroy its beneficial properties. In addition to this, try to buy and store nuts, seeds and their oils in small quantities to ensure that they are as fresh as possible and limit the amount of time the oils have to degrade.
It is difficult to say exactly how much of a certain food should be consumed to optimise EFA intake as the fatty acid content of foods varies. However, a sensible approach is to reduce consumption of omega-6 rich vegetable oils (substitute sunflower or corn oil for olive oil in cooking), while increasing omega-3 intake (found in flaxseed oil, walnuts and green leafy vegetables). Limiting or avoiding commercial oil-based processed foods will also help improve the omega-6:omega-3 ratio. Consumption of saturated fatty acids (and trans fatty acids in processed foods) should also be limited as they are unnecessary in the diet, are a risk factor for atherosclerosis and can interfere with the conversion of ALA into the longer chain omega-3s.
To improve the conversion of ALA to EPA and DHA follow these simple guidelines:
- Consume a wide range of wholefoods everyday – remember variety is the spice of life!
- Obtain most fat from whole foods (nuts, seeds, wholegrains, olives, avocados and soya)
- Select monounsaturated fat (olive oil) for cooking
- Use omega-6 fats (sunflower oil, safflower oil) with moderation
- Use omega-3 fat (flaxseed oil) for salad dressing and in dips but do not cook with it (store it in the fridge)
- Cut down on cholesterol (avoid eggs, meat and dairy products)
- Avoid or cut down on processed foods, trans fats from margarines and hydrogenated vegetable oils
- Avoid or reduce fried foods, alcohol, caffeine, sugar, smoking and stress
No short cuts, no magic bullet…
Fish is not a health food. Neither is it a magical wonder food that can guarantee good heart health and turn all kids into geniuses. The real problem here is not just the lack of good fats in the diet; it’s the generally appalling state of most people’s diets. Fish is not a popular food; on average people in the UK eat only a third of a portion of oily fish per week with seven out of ten people consuming none whatsoever. We should stop looking for a ‘quick miracle fix’ and focus on the bigger picture. improving our diets by cutting out the saturated fatty foods laden with animal fats, sugar, salt and cholesterol and eating more fruit, vegetables, pulses, whole grains, nuts and seeds.
This report explains what the current research shows: fish may be a source of protective fats but they are not the only, nor the healthiest, source. Fish are also a source of unhealthy and unnecessary saturated fat in the diet. Plant-derived EFAs are a far superior source of good fats in the diet.
Environmental contamination of the oceans now means that when you take a mouthful of fish you are also taking a mouthful of neurotoxins and carcinogens (mercury, PCBs and dioxins). Some people might consider this game of Russian roulette worth the risk if the health benefits afforded from fish could not be gained elsewhere. However, the research clearly shows that ALA from plants can protect heart health and doesn’t come laced with poison. Plant-derived EFAs have numerous advantages over fish-derived fats yet are virtually ignored by health professionals. This may be due to the paucity of relevant research. The VVF is trying to address this by pushing for more research including plant-derived ALA alongside the fish oils EPA and/or DHA.
Including fish in the typical Western diet, high in saturated and processed fat, will not provide the health benefits that many people seek. A far more effective way to achieve good health is to adopt a more plant-based diet low in saturated fat and cholesterol but containing a healthy amount of polyunsaturated EFAs. Well-balanced vegetarian and vegan diets, containing EFA-rich foods, not only help combat heart disease but also protect against many other degenerative diseases.
Although the main focus of this report is human health, the environmental argument for switching to plant-based omega-3s cannot be ignored. We know how commercial fishing is devastating the world’s oceans and fish stocks are plummeting. Flaxseed and other plant-based sources of omega-3s are sustainable sources of this important fatty acid as well as being the healthier option. The many arguments supporting the move towards plant-based omega-3s away from fish oils are indisputable.
Our hearts don’t need fish, our brains don’t need fish and our health is far better served by plant EFAs as part of a well-balanced plant-based diet. Next time you are told of the magical properties of fish oil, you’ll know what to say… fish is not a health food.