Covid-19 – what you need to know

Covid-19 caused a global health emergency and wreaked havoc across the world. It shut down entire countries and pushed healthcare services to unprecedented limits.
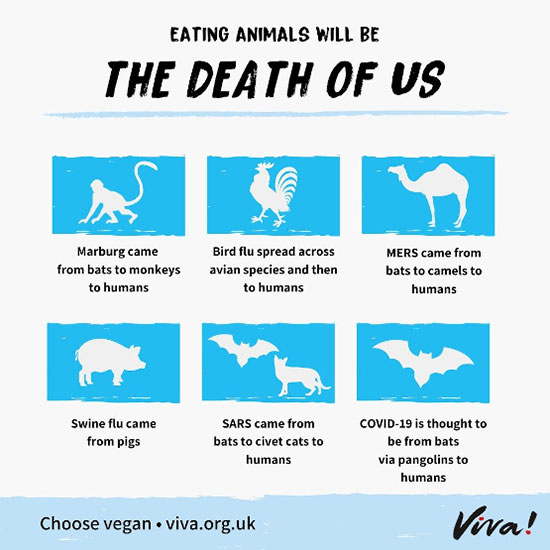
Covid-19 is one more disease in a long line of zoonotic diseases – SARS, MERS, bird flu, Ebola and AIDS to name a few – which come from the exploitation and consumption of animals. Three-quarters of the world’s new or emerging infectious diseases come from animals, mainly from trading in wildlife and from factory farming. Taken together, 56 zoonotic diseases are responsible for an estimated 2.5 billion cases of human illness and 2.7 million deaths a year.
In the wake of Covid-19, there are calls for tighter controls at airports, banning the unregulated movement of wild animals and limiting human-animal contact. But the obvious solutions, the simplest, most economical and effective solutions, are to end the global trade in wild animals and to stop eating animals.
Here, we answer the most frequently asked questions about Covid-19 and explain why we must stop eating animals to prevent future pandemics.
Our 3 in 4 campaign
Three in four of the world’s new or emerging infectious diseases come from animals. Responsible for nearly three million deaths a year, these diseases are largely transmitted through trading wildlife (legally and illegally) and factory farming.
Our Slash the Risk Campaign
Our Slash the Risk campaign placed huge billboards in the West Midlands and Bristol in November and December of 2020 which reached over 12 million people. One revealed the risk from factory farming and urged people to try Viva!’s new V7 challenge to go vegan for one week; while another urged people to protect themselves from severe Covid symptoms by going vegan.
A virus is an infectious agent that can only replicate itself within a host organism, using the host’s cells to produce copies of itself. They can infect many different organisms, including bacteria, plants (although not coronaviruses) and animals – including humans.
Viruses are so small that their existence wasn’t realised until the 1890’s and were first seen only in 1939 following the introduction of the electron microscope. Viruses are extremely small and the jury is still out as to whether or not they are living organisms. Their genetic material (viral genome) is contained within a protein shell called a capsid and can vary greatly – they can be DNA or RNA, single or double-stranded, linear or circular, and vary in length and in the number of DNA or RNA molecules. In some viruses, the protein shell is enclosed in a membrane called an envelope.
They do it in order to replicate themselves as they cannot reproduce in any normal way that we can relate to.
A virus infects its host by attaching to one of the hosts cells and penetrating the cell wall or membrane. The virus’s genome is uncoated from the protein shell and injected into the host cell where it hijacks its machinery, forcing it to replicate the viral genome and so producing component parts for new viruses which are then assembled into complete viruses. These new viruses then burst out of the host cell in a process called lysis, which kills the host cell. The new viruses may then go on to infect new cells and ultimately new hosts.
Many diseases in humans are caused by viruses, such as influenza, chicken pox, German measles, AIDS, Ebola, the common cold and rabies. The primary defence against viral infections is vaccination made up of inactive viral particles which act as antigens and alert the body’s immune system in much the same way as an active virus would. The body’s immune system responds by producing antibodies that fight the invader and increase its immunity to the disease.
The major health problem with viral infections is that it is very difficult to destroy the viruses without destroying our own human cells that harbour them.
Bacteria are much larger than viruses, were first discovered in 1676 and can been seen under a normal microscope. They are single-celled organisms that can thrive in a range of environments – soil, oceans, plant and animal cells and for some bacteria that includes human cells, in fact almost anywhere – and can reproduce without invading our cells.
Bacteria were among the first life forms to appear on Earth, and are present in almost all the life forms that subsequently developed – in fact, they couldn’t live without bacteria. That relationship can be symbiotic (to the benefit of both the bacteria and host) or parasitic (the bacteria lives off the host). A good example of a symbiotic relationship in humans is the ‘good’ bacteria in our intestines which extract energy from food, create vitamins and amino acids and form barriers against infective invaders. They even stimulate your immune system, break down toxins and boost your overall health. So not all bugs are bad! There are typically 40 million bacterial cells in a gram of soil and a million in a millilitre of fresh water.
Before the Second World War, the main causes of death across the world were bacterial infectious diseases such TB, pneumonia and cholera. With the widespread introduction of antibiotics after the war, these and other infectious diseases could be successfully cured but antibiotics are ineffective against viruses. In developed countries, the main cause of death became degenerative diseases caused by diet and lifestyle – heart disease, obesity, diabetes, strokes etc.
The overprescribing of antibiotics and particularly their use in farmed animals, which accounts for 75 per cent of all antibiotics worldwide, has seen their effectiveness diminish and bacterial infectious diseases, which were believed to have been defeated, are beginning to appear once more. Worryingly, no new antibiotic has been discovered since 1980 and, even more worrying, no new class of antibiotics has been discovered since 1962.

Coronaviruses are a large family of viruses which can cause illness in animals and humans. In humans, several coronaviruses are known to cause respiratory infections, ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) and the most recent, Covid-19, caused by a new coronavirus that emerged in China in 2019.

Many of the most virulent diseases that infect humans have been transmitted to us from animals. In fact, a whopping 75 per cent of new or emerging infectious diseases in people come from animals, according to the Centers for Disease Control and Prevention.
Before humans started farming animals none of the major infectious diseases affected us but we now know that whooping cough came from pigs, typhoid fever from chickens, influenza from ducks, leprosy from water buffalo and the common cold from horses.
As we then crammed ever-more animals together in ever-more filthy and unhygienic conditions such as in factory farms, we have begun a game of pandemic Russian roulette.
Placing humans in ever closer contact with animals has enabled their diseases to mutate and infect us. Bats, civet cats, pangolins, wolf pups, beavers and many other forms of wildlife are on sale all over China and beyond in ‘wet’ markets, either slaughtered to order or to take away to kill. The deadly SARS coronavirus outbreak in 2003 was traced directly to a colony of horseshoe bats but it was farmed wildlife – civets in this case – that were sold for food and Chinese medicine (they are believed to improve male virility, among other health attributes), that acted as a vector to pass the virus to humans.
The terrifying Ebola disease has been traced to eating primates (as bushmeat) who had been infected by bats. Bats were also involved in MERS and are believed to have spread the disease via camels, although the camel showed no symptoms.

Again, wild animals and wet markets are thought to be involved. Several independent research groups have confirmed that SARS-CoV-2 coronavirus is very similar to a bat coronavirus, indicating bats as the natural host.
Genomic comparisons suggest that the SARS-CoV-2 virus (the cause of COVID-19) is the result of a recombination between two different viruses. In other words, it is thought to be a mix of pre-existing viruses in bats and another animal, possibly brought together at the Huanan Seafood Wholesale Market in Wuhan, China. Here, wild animals, including birds, bats, pangolins, rabbits, bats, marmots and snakes were traded.
However, it is also possible the virus emerged a little earlier and again scientists state that the cause is trading in wild animals. Georgetown University infectious disease specialist Daniel Lucey states that the animal-to-person transmission of the virus could have occurred “in one or more multiple markets, or restaurants, or farms, or with wild animals, legal or illegal trade.”
Coronaviruses are known to jump from animals to humans, so it’s thought that many of the first people infected with the disease (mainly stallholders from the seafood market) contracted it from contact with animals. It then spread from human to human.
The important point is that destroying and eating animals is destroying everything, including us!

After 20 years of severe food shortages and famine, the Chinese government abandoned collective farming and in the late 1970s encouraged farmers to trap wild animals including civets, snakes, rats, peacocks, porcupines, bats and many more species to commercially breed them for food.
Unfortunately, there are also cultural beliefs that wild animal parts, such as pangolin scales and bear bile, used in traditional Chinese medicine cure many ailments and make men more sexually virile. In June, 2020, Chinese authorities took pangolin scales off the Chinese pharmacopoeia, an official list of medicines and ingredients approved for use. The Chinese State Forestry and Grassland Administration (SFGA) has also raised the protected status of pangolins to the highest level, with strict penalties on those caught killing or trading them.
Since the mid-1980s, China has modernised its farming of animals with vast factory farms (China is the world’s largest pork consumer, slaughtering almost 700 million pigs in 2021). So now the trade in wild animals runs alongside factory farming, two perfect storms for creating pandemics.
The outbreak of Covid-19 revealed the scale of China’s trade in wildlife, both legal and illegal. A temporary ban covered some 20,000 wild animal breeding facilities and 54 species that were traded legally. A report by the Chinese Academy of Engineering estimates the wildlife farming industry is worth around US$57 billion annually. These breeding centres were allowed to operate under loopholes in Chinese domestic law, against the spirit of the Convention on International Trade in Endangered Species of Wild Fauna and Flora (CITES). The parallel illegal trade is less easy to quantify, but globally it is valued by the UN at US$23 billion.

In February 2020, the 16th meeting of the Standing Committee of the 13th National People’s Congress in China on ‘Comprehensively Prohibiting the Illegal Trade of Wild Animals, Eliminating the Bad Habits of Wild Animal Consumption, and Protecting the Health and Safety of the People,’ permanently banned all trade and eating of terrestrial wild animals, whether captive-bred or wild-caught. Many scientists welcomed the new law, which was finalised in December 2022. It “clearly prohibits the consumption, hunting, trade and transport of terrestrial animals that grow and breed naturally in the wild,” says Jiahai Lu, an epidemiologist at Sun Yat-Sen University, Guangzhou.
Although potentially a huge step forward, the rules also have worrying weaknesses. According to an analysis by the Wildlife Conservation Society, the decision does not ban trade for fur, zoos, pets, traditional Chinese medicine, conventional medicine or research. This creates a potential loophole for traffickers who may exploit the non-food exemptions to sell or trade live wildlife. The rules permit, for example, farmers to raise raccoon dogs and other mammals for their fur—fuelling concerns that the farms could promote the emergence of new human diseases. In March 2023, for example, researchers released an analysis of genetic material collected at the Huanan Seafood Wholesale Market in Wuhan, that suggests raccoon dogs and other wildlife being sold illegally at the market were carrying SARS-CoV-2.

SARS-CoV-2 (that causes Covid-19) is the seventh coronavirus known to infect humans. SARS-CoV, MERS-CoV and SARS-CoV-2 can cause severe disease, whereas the other coronaviruses HKU1, NL63, OC43 and 229E are associated with mild cold symptoms.
SARS: Emerged 2002. There have been two SARS outbreaks, which resulted in a highly contagious and potentially life-threatening form of pneumonia. Both happened between 2002 and 2004. During the period of infection, there were 8,098 reported cases of SARS and 774 deaths. Death rate: 10%
MERS: Emerged 2012. From April 2012 to October 2022, a total of 2,600 laboratory-confirmed cases of MERS were reported globally, with 935 deaths. The majority of cases were reported from Saudi Arabia, with 2,193 cases and 854 related deaths. Death rate: 36%
Covid-19: Emerged 2019. Over 600 million cases of Covid-19 have been reported globally (very many cases are not tested for or reported in some countries, so the true figures are much higher). At the end of September 2020, global coronavirus deaths passed one million and as of April 2023, global deaths have now exceeded seven million and over 230,000 people have died in the UK. See the WHO dashboard here for the latest figures. Death rate: between 0.7 and 3.4%. Estimated at 3.2% by the World Health Organisation in March 2020. Countries with more elderly populations or with fewer people vaccinated will have higher rates.
The virus is called SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) and the disease it causes is called Covid-19, a shorter version of ‘coronavirus disease 2019’.
Most viruses have lived for millennia in wild animals without harming them, allowing the viruses to replicate without killing their host – which, would of course kill the viruses, too. By their nature, viruses constantly mutate, and these mutations may find other, different hosts. In fact, the extremely high mutation rates of viruses are not matched by any organism in the kingdom of life. The high mutation rates of viruses, coupled with short generation times and large population sizes, allow viruses to rapidly evolve and adapt to the host environment.
That is what happened with Covid-19 – it is a virus that has not infected humans before and that is one reason why it is so highly contagious – we have little or no residual resistance. The other reason is bad luck – two viruses swapped particular genes that make the new or novel form able to pass from person to person with ease, though its death rate is relatively low, between 0.7 and 3.4 per cent (depending on the location and, crucially, access to vaccines and good hospital care).
Whereas, with MERS and SARS, although not as contagious as Covid-19, they are much more deadly, killing around 34 and 10 per cent respectively. The World Health Organisation say the mortality rate for the avian influenza virus H5N1 is about 60 per cent, thankfully it does not spread between humans easily. It is a matter of time before a pandemic breaks out where the worst happens: fiercely contagious and very deadly.
The main symptoms of coronavirus initially were:
- a high temperature – this means you feel hot to touch on your chest or back
- a new, continuous cough – coughing a lot for more than an hour, or three or more coughing episodes in 24 hours
- a loss or change to your sense of smell or taste – this means you’ve noticed you cannot smell or taste anything, or things smell or taste different to normal
The top five symptoms of the Omicron variant (according to the ZOE COVID study) are:
- runny nose
- headache
- fatigue (mild or severe)
- sneezing
- sore throat
Common symptoms of Covid-19 are fever, tiredness and dry cough. Some people may have aches and pains, nasal congestion, runny nose, sore throat or diarrhoea, although these are mild and begin gradually. Some people become infected but don’t develop any symptoms and don’t feel unwell and most (about 80 per cent) recover from the disease without needing special treatment.
Older people and those with underlying medical problems such as obesity, high blood pressure, heart problems or diabetes, are more likely to develop serious illness. People with fever, cough and difficulty breathing should seek medical attention.
A large number of people are reporting symptoms that last for weeks or months. While Covid-19 can cause a period of acute illness, some people continue to experience symptoms, such as breathlessness, muscle aches and fatigue, for weeks, months or even years – a condition that has been called long Covid.
Chest pains, shortness of breath and fatigue are among the commonly described symptoms along with ‘brain fog’ and a loss of smell and taste. Some people experience lasting damage to their heart and lungs and blood clots that can cause painful swelling or strokes. Estimates suggest that there could already be millions of people around the world living with long Covid and in the UK, figures from the Office for National Statistics (ONS) reveal that as many as two million people living in the UK (3.1% of the population) reported they were still experiencing Covid symptoms more than four weeks after their first suspected coronavirus infection.
Although a small number of people end up in hospital, the vast majority of people who get Covid-19 are either asymptomatic or suffer a mild illness, are not hospitalised and do not require oxygen. Of those who do go to hospital, around half develop complications. A large-scale study published in The Lancet has found that one in two people hospitalised with Covid-19 earlier in the pandemic, before vaccines were available, developed at least one health complication.
They looked at more than 70,000 adult patients in the UK hospitalised with severe Covid-19 between January and August 2020. Of these, half developed one or more health complication. The most common of these included:
- renal (24%)
- respiratory (18%)
- systemic (16%)
- cardiovascular (12%)
In addition, neurological, gastrointestinal and liver complications were also reported. The most common problems experienced by patients were kidney damage, acute respiratory distress syndrome, liver injury, anaemia and cardiac arrhythmia (irregular heartbeat).
There were a high proportion of complications in Covid-19 patients across all age groups dispelling suggestions that Covid-19 presents no risk to younger healthy adults, many of whom remain unvaccinated.
Although people over 60 were most likely affected, complications were common, even in younger, previously healthy adults. They found that 27 per cent of 19 to 29-year-olds and 37 per cent of 30 to 39-year-olds experienced a complication. These figures rise to 54 per cent of 60 to 69-year-olds and to 52 per cent for people in their 80s.
One in eight of the youngest group, aged 19 to 29, suffered acute complications which meant that they were unable to look after themselves after being discharged from hospital.
Dr William van’t Hoff, Chief Executive of the NIHR Clinical Research Network said: “The work, performed in the first phase of the pandemic, underlines how serious Covid-19 is and reinforces the importance not only of the treatments now available, but critically, the role of vaccination in reducing infection and lessening its impact.”
You can catch Covid-19 from others who have the virus. The disease can spread from person to person through small droplets from the nose or mouth which are spread when an infected person coughs, sneezes or exhales. These droplets land on objects and surfaces around the person and other people can then catch Covid-19 by touching these objects or surfaces, then touching their eyes, nose or mouth.
People can also catch it if they breathe in droplets from a person with Covid-19 who coughs out or exhales droplets – and this is why it is important to stay more than two metres (over six feet) away from anyone during a period of self-isolation.

The main way the disease spreads is through respiratory droplets expelled by someone who is coughing. The risk of catching Covid-19 from someone with no symptoms at all is probably very low. However, many people with Covid-19 experience only mild symptoms – particularly during the early stages of the disease. If that person does not feel ill but has a mild cough, it is possible to catch it from them. Research is still taking place on this by the World Health Organisation (WHO).
The risk of catching the disease from the faeces of an infected person appears to be low but theoretically possible. While the virus is certainly present in faeces in some cases, this is not the main route of transmission but the faeces-oral route is thought to exist and causes gastro-intestinal symptoms. It is another reason to thoroughly wash your hands before meals and after going to the toilet.
Yes, but more to protect others. Wearing masks almost entirely prevents tiny droplets from the mouth from spreading the virus.
Countries that mandated the wearing of masks initially reduced the cases of Covid-19 considerably. For example, the Czech Republic had made home-made masks as a community effort, which helped effectively reduced the spread. On 14 April 2020, there were 11,329 deaths caused by coronavirus in the UK; and 143 in the Czech Republic. This translates to 167 deaths/1 M pop in the UK compared to 13 deaths/1 M pop in the Czech Republic. Canada and South Korea also require or advise their citizens to wear masks in public places. And the US Centers for Disease Control and Prevention (CDC) now advises the wearing of cloth masks in public.
Although the numbers of infections have risen around the world, most authorities continue to recommend using face-covering and masks in public places. Masks help stop the spread as people who are infected with coronavirus may not show symptoms for several days, and so do not know they are infected. When we speak, micro-droplets are emitted from our mouths, masks – including homemade ones – stop most of the droplets from being ejected.
The masks offer less protection from catching the virus (if the infected person wasn’t wearing a mask) because after the droplets have been emitted from the mouth, they dry out and turn into droplet nuclei which are very tiny and harder to filter.
So masks are about protecting the community. Prof David Heymann CBE, a World Health Organization (WHO) adviser, said, “I think that wearing a mask is equally effective or more effective than distancing.” As there is a worldwide shortage of masks and as healthcare workers come first, it’s time to get imaginative and make your own! The Centers for Disease Control and prevention offers advice here on wearing homemade masks.
Other effective ways to help protect yourself and others against Covid-19 are to frequently wash your hands with plenty of soap and water for 20 seconds, cover your cough with the bend of an elbow or tissue and maintain a distance of at least two metres (six feet) from people who are coughing or sneezing.

On average it takes five to six days from when someone is infected with the virus for symptoms to show, however it can take up to 14 days. These estimates may be vary with new variants.
Almost 60 species of mammal are thought to be susceptible to SARS-CoV-2. So far, the ones we know are, include: cats, dogs, ferrets, lions, tigers, gorillas and mink. A number of companion animals (cats and dogs) have been infected with the virus in several countries, becoming sick after being in contact with an infected person. To date, there is no other evidence that any dog, cat or other companion animal have infected humans. In September 2021, more than a dozen gorillas tested positive for Covid-19 at a zoo in Atlanta, Georgia in the US, probably after contracting the virus from a keeper, it is thought. In 2022, hundreds of white-tailed deer in North America tested positive for SARS-CoV-2. It’s not yet clear whether deer-to-human transmission could spark outbreaks but scientists are growing increasingly concerned about animals becoming viral reservoirs potentially breeding new variants.
The CDC says that animals may become infected after contact with people with Covid-19. Animals reported infected include:
- companion animals, including cats, dogs and ferrets
- animals in zoos and sanctuaries, including several types of big cats, otters and non-human primates
- mink on mink farms
- wild white-tailed deer in several US states
Mink have both caught the virus from people and transmitted it back to them. They can act as a reservoir for the virus and mink fur farms have provided the perfect environment for the virus to mutate and then spread back to humans raising concerns that the mutated version (or variant) might be even more deadly or may hamper the development of a vaccine. Since June 2020, 214 human cases of Covid-19 have been identified in Denmark with SARS-CoV-2 variants associated with farmed minks, including 12 cases with a unique (mutated) variant.
At the moment, there is no evidence that the mutated version is more dangerous or that it would diminish the value of vaccines currently in development. However, the human-mink-human transmission shows the real danger of what virologists call ‘reverse spillover’ and demonstrates what a potential danger factory farms pose.
There is some uncertainty about how long Covid-19 can survive on different surfaces but it seems to behave like other coronaviruses. Studies on these have shown that the virus may persist on surfaces for a few hours or up to several days. (However, the virus degrades outside of the host’s body and so quickly becomes less able to infect a new host.) This may vary according to the conditions, type of surface, temperature and humidity.
The virus may live longer on harder surfaces such as plastic, glass and steel and shorter on softer surfaces such as fabrics, paper and cardboard. (This is because the virus is more stable within warm, moist environments like our body! Absorbent materials suck moisture away from the virus, causing their structure to collapse.) Wiping down hard surfaces with simple disinfectant is capable of destroying Covid-19. And remember to wash your hands often.
The likelihood of an infected person contaminating commercial goods is low and the risk of catching the virus from a package that has been moved, travelled and exposed to different conditions and temperature is also low. It isn’t just about the virus being present but about the ‘viral load’ – it has to present in sufficient quantity to transmit the infection and for the structure to be intact. It would be good practice to wash your hands after taking delivery of a package if you are concerned.
Sunbathing and temperatures over 25°C offer no protection – you can catch Covid-19 no matter how sunny or hot the weather and countries that do have hot weather have reported cases of the virus. Similarly, claims that hot and humid weather can cause its transmission are also untrue and taking hot baths offers no protection. The normal human body temperature remains around 36.5°C to 37°C, regardless of the external temperature or weather.
There is also no reason to believe that cold weather can kill the new coronavirus.
Pandemics often don’t follow the same seasonal patterns seen in more normal outbreaks. It is true that eventually, we would expect to see Covid-19 becoming endemic and seasonal. Jan Albert, a professor of infectious disease control who specialises in viruses at the Karolinska Institute in Stockholm, says once Covid-19 is endemic, “it would be really surprising if it didn’t show seasonality then. The big question is whether the sensitivity of this virus to [the seasons] will influence its capacity to spread in a pandemic situation. We don’t know for sure”.
No, and frequent or excessive alcohol consumption can increase your risk of other health problems.
There is no evidence to suggest that the virus can be transmitted by mosquitoes. It is a respiratory virus which spreads primarily through droplets generated when an infected person coughs or sneezes, or through droplets of saliva or discharge from the nose.
No. Hand-dryers are not effective but they are very efficient at blowing other possible infections around the room. It is best to dry your hands with disposable paper towels.
UV lamps should not be used to sterilise hands or other areas of skin as UV radiation can cause skin irritation.
No. Spraying alcohol or chlorine all over your body will not kill viruses that have already entered your body. Spraying such substances can be harmful to clothes or mucous membranes such as eyes, nose and mouth. Both alcohol and chlorine can be useful to disinfect surfaces but they need to be used according to the recommendations.
See our vaccine fact sheet: viva.org.uk/materials/vaccines-factsheet
Covid-19-vaccines can protect you from getting and spreading the virus that causes Covid-19. If you do get it, the vaccine may help prevent you from getting seriously ill and needing hospitalisation and oxygen support. Although older people are more likely to be seriously ill, some younger people have been very ill too and many have been affected by long Covid.
However, it’s important to remember that it’s not only about you. When large numbers of a population are immunised, it reduces the risk of exposure for everyone in the community including vulnerable people who are ill or have a weakened immune system. This is called ‘herd immunity’ and requires most people to opt in for it to be effective. By getting vaccinated you are protecting people around you, particularly those at increased risk for severe illness from Covid-19. Therefore, you will be protecting others by getting the vaccine.
Studies show that the AstraZeneca, Pfizer and Moderna vaccines are effective against the Delta and Omicron variants. Although they may not always prevent you from catching Covid-19, they appear to be highly effective at preventing hospitalisation and death from it and may lower the risk of you spreading it. Opting out of vaccination programmes increases the risk of outbreaks. So while some see vaccination as a personal choice, there is a social responsibility too – protecting yourself and your community.
No. There is no evidence that regularly rinsing the nose with saline has protected people from infection with the new coronavirus.
Garlic is a healthy food that has some antimicrobial properties but there is no evidence that it has protected people from the current outbreak.
Even though we don’t understand everything about coronavirus Covid-19 just yet, we know that certain people are at a higher risk from it. Their immune system may be compromised or they have a condition that makes it more likely for coronavirus infection to put their lives in danger. In Italy, 99 per cent people who died had at least one underlying condition.
Covid-19 is more dangerous for older people simply because as we age, our immune system gradually weakens. There isn’t much we can do about aging but ensuring good nutrition is important for our immune system to be at its best.
Heart disease and diabetes are the two main underlying conditions that seem to make matters much worse regardless of age. The good news is that both can be prevented and even reversed through diet. Heart disease, high blood pressure and cholesterol respond really well to wholesome vegan diets, so much so that in some trials, they were more effective than medication. Type 2 diabetes has also been studied extensively and a low-fat vegan diet based on wholefoods has achieved great success in a number of studies.
Asthma sufferers are seen as vulnerable to Covid-19 complications because the infection affects the airways and can trigger serious asthma attacks. The condition also increases likelihood of pneumonia and acute respiratory stress. Asthma cannot be treated but research shows that a diet high in antioxidants from fruit and vegetables can help reduce airway inflammation.
Cancer is another disease that puts people at high risk from Covid-19 complications. It not only compromises the immune system and causes a host of health issues but patients may also struggle to access their much-needed treatment and medications at this time. We cannot cure cancer with diet but a healthy lifestyle can help prevent it or support the treatment.
Chronic kidney disease has been linked to an increased risk of coronavirus infection progressing to the life-threatening pneumonia stage. Wholesome vegan diets have a kidney-protective effect, while animal-based ones can cause harm and kidney patients are actively advised against eating meat.
Several other factors, such as smoking and excessive alcohol consumption, and conditions, such as liver disease, HIV/AIDS and severe obesity also increase the risk of life-threatening complications. While we cannot entirely protect ourselves from infection, there’s always room for improvement when it comes to our lifestyle habits!
Find out how to Slash your risk of severe Covid-19.
Two studies show that not only does a plant-based diet lower the risk of severe Covid-19, but it may also lower your risk of getting it.
The first study, published in the BMJ Nutrition, Prevention & Health journal, confirmed what Viva! were saying for months – a vegan diet may slash your risk of severe Covid-19.
The study included people from France, Germany, Italy, Spain, UK and USA who were infected with Covid-19. Their diet and symptoms were recorded and analysed to reveal that those who followed a plant-based diet were 73 per cent less likely to experience moderate-to-severe Covid symptoms.
The ZOE COVID Symptom Study, the largest study to date looking at diet and Covid, found that those on a plant-based diet are 10 per cent less likely to get Covid, and if they do, they are 40 per cent less likely to require hospitalisation and oxygen support.
The advantage of being vegan may come from the lower rates of underlying conditions that have been shown to increase the risk of coronavirus infection turning deadly – heart disease, type 2 diabetes, kidney disease, obesity, cancer and chronic lung disease. Vegan diets also lead to beneficial gut bacteria that produce health-supportive substances and may help strengthen the immune system. They are also packed with vitamins, minerals and disease-busting antioxidants.
See what you should eat each day for good health.
In England and Wales, between March 2020 and March 2022, the Office for National Statistics said that most (58.3 per cent) deaths due to Covid-19 occurred among those aged 80 years and over. Around one in three (33.8 per cent) occurred among people aged 60 to 79 years, 7.9 per cent were among those under 60 and the youngest age group (those aged up to 14 years) accounted for just 0.03 per cent of deaths due to Covid-19.
The overall case fatality rate (CFR) reflects the number of deaths divided by the number of diagnosed cases within a given time interval. Based on Johns Hopkins University statistics, the global death-to-case ratio is 1.02 per cent as of March 2023. The number of deaths due to Covid-19 has generally remained higher across all age groups than the number of deaths due to seasonal flu.
People of all ages can be infected but older people and those with pre-existing medical conditions, such as obesity, high blood pressure, asthma, diabetes and heart disease, appear to be more vulnerable than others. Men have a higher risk than women and black, Asian and minority ethnic (BAME) people have a higher risk than white ethnic groups.
It has been widely reported that children are much less likely to get severely ill and die from the new coronavirus. This may be because children’s immune systems are still developing, so they are shielded from a dangerous immune response – called a cytokine storm – where the immune response against the coronavirus becomes overzealous and causes life-threatening damage to the lungs.
Covid-19 fatality rate by age:
*Death Rate = (number of deaths/number of cases) = probability of dying if infected by the virus (%). This probability differs depending on the age group. The percentages shown below do not have to add up to 100%, as they do NOT represent share of deaths by age group. Rather, it represents, for a person in a given age group, the risk of dying if infected with Covid-19.
| AGE | DEATH RATE confirmed cases | DEATH RATE all cases |
|---|---|---|
| 80+ years old | 21.9% | 14.8% |
| 70-79 years old | 8.0% | |
| 60-69 years old | 3.6% | |
| 50-59 years old | 1.3% | |
| 40-49 years old | 0.4% | |
| 30-39 years old | 0.2% | |
| 20-29 years old | 0.2% | |
| 10-19 years old | 0.2% | |
| 0-9 years old | 0.006% |
All viruses mutate, this is why a new flu vaccine is produced each winter to tackle the constantly changing threat posed by flu viruses.
There have been concerns that the SARS-CoV-2 coronavirus, responsible for Covid-19, could evolve to become more dangerous. The virus is being constantly monitored to see if any significant changes occur.
Many different mutations have been spotted but none were thought to have much significance until September 2020, when a new variant was detected in the UK. This became known as the Kent variant but is now referred to as the Alpha (B.1.1.7) variant. It was found to be more transmissible and soon became the dominant variant in the UK.
The Beta (B.1.351) variant was first detected in South Africa and led to an increase in hospitalisations there as cases rose. The Gamma variant (P.1), first detected in the US in January 2021, was also found to spread more easily than its predecessor.
The Delta (B.1.617.2) variant was initially detected in India but fast became the dominant variant in the UK. Initial studies suggested that it may be up to 70 per cent more transmissible than the Alpha variant. Evidence also suggests that it may also cause more severe disease in people who are not vaccinated. The Delta variant is associated with approximately double the risk of hospitalisation compared with the Alpha variant. However, the vaccines designed to tackle Covid-19 still appear to be effective, at least for now.
The Omicron variant (B.1.1.529) was first reported to the World Health Organisation from South Africa on 24 November 2021. This variant has an unusually large number of mutations which appear to make it even more transmissible than Delta but some evidence suggests it may be less dangerous than the Delta variant. By the end of 2021, Omicron cases constituted more than 90 per cent of all Covid-19 cases in England.
Most people will probably get Covid-19 many more times. The good news is that, when reinfection does occur, the immune system seems primed to respond. Evidence is building that there is a lower risk of severe or fatal outcomes with reinfections than with the first bout. But repeat infections are not harmless: there are cumulative risks and repeated SARS-CoV-2 infections are especially dangerous to the most vulnerable. For those with long Covid, studies suggest that reinfection can exacerbate the symptoms, although the chances of getting it in the first place diminish with subsequent infections.
Zoonoses: a ticking time bomb
Read our report, written by Viva!’s Dr. Justine Butler on emerging diseases originating in animals and their impact on humans.

From a Bat Out of Hell
Juliet Gellatley, founder of Viva! and zoologist, explores the animal origins of coronavirus.

The Viva! Vegan Podcast - #42 April 2020
Hear about Covid-19 from a different perspective than you’re hearing on mainstream news. Juliet Gellatley is joined by Viva!’s Associate Director, Tony Wardle, in a detailed conversation about how the virus started, its connections to factory farming, the role of veganism and what this means for the future.
Listen to the conversation below and then share the full podcast here.


This content was written by Juliet Gellatley, and reviewed by Dr Justine Butler.
Tags: Coronavirus, Covid-19, Zoonoses