Simple Tips to Sharpen Wits Factsheet
Health Charity Viva!Health Suggests Ten Clever Reasons to Go Vegan!
1. Folic Acid Boosts Brain Power
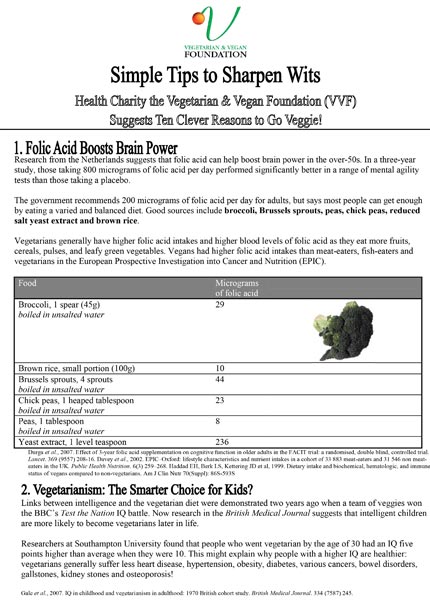
Research from the Netherlands suggests that folic acid can help boost brain power in the over-50s. In a three-year study, those taking 800 micrograms of folic acid per day performed significantly better in a range of mental agility tests than those taking a placebo.
The government recommends 200 micrograms of folic acid per day for adults, but says most people can get enough by eating a varied and balanced diet. Good sources include broccoli, Brussels sprouts, peas, chick peas, reduced salt yeast extract and brown rice.
Vegetarians generally have higher folic acid intakes and higher blood levels of folic acid as they eat more fruits, cereals, pulses, and leafy green vegetables. Vegans had higher folic acid intakes than meat-eaters, fish-eaters and vegetarians in the European Prospective Investigation into Cancer and Nutrition (EPIC).
2. Vegetarianism: The Smarter Choice for Kids?
Links between intelligence and the vegetarian diet were demonstrated two years ago when a team of veggies won the BBC’s Test the Nation IQ battle. Now research in the British Medical Journal suggests that intelligent children are more likely to become vegetarians later in life. Researchers at Southampton University found that people who went vegetarian by the age of 30 had an IQ five points higher than average when they were 10. This might explain why people with a higher IQ are healthier: vegetarians generally suffer less heart disease, hypertension, obesity, diabetes, various cancers, bowel disorders, gallstones, kidney stones and osteoporosis!
3. Bolster your Mood
Shorter days and low light levels can trigger winter depression, or Seasonal Affective Disorder (SAD). SAD sufferers tend to crave sweet or starchy foods, which are natural short-term mood improvers. These foods naturally cause the brain to produce a chemical called serotonin – the same brain chemical that is elevated by antidepressants. According to Dr Neal Barnard, author of Breaking the Food Seduction (St Martin’s Griffin, New York), there is nothing wrong with using these foods to cope with the winter blues. Just choose them carefully – especially if you don’t want to put on weight. “Biscuits, cakes and chocolate contain plenty of carbohydrate (which is not likely to cause much weight gain all by itself), but they also contain enough butter. or other fats to add a lot of calories. In contrast, wholegrain bread, brown rice or rice cakes, pasta and fruit provide healthful carbohydrate, which increases your natural serotonin production with very little fat – as long as you don’t add it in the kitchen.” Dr Barnard adds: “Winter depression – and the overeating that comes with it – also responds well to daylight, especially a generous amount of it early in the morning.” He recommends a 20-minute walk outdoors in the first morning light to help cut food cravings and to boost mood and energy levels.
4. Cut Dementia Risk
Research in the British Journal of Medicine suggests that being obese during your forties can increase your risk of developing dementia. Detailed health checks were made on over 10,000 men and women between 1964 and 1973 (when they were aged 40 to 45). Seven per cent of participants went on to develop dementia. Being obese increased dementia risk by 74 per cent, while being overweight increased it by 35 per cent. The link between obesity and dementia in women was stronger than that in men.
These findings concur with a Swedish study which found that the higher a woman’s body mass index (BMI), the greater her risk of dementia. The 18-year study assessed 392 adults between the ages of 70 and 88. Of the 93 participants diagnosed with dementia, women who developed it had a higher average BMI than those who didn’t. For every one unit increase in BMI at age 70 years, the risk of dementia increased by 36 per cent. A wealth of research suggests that vegetarians and vegans have a lower risk of overweight and obesity and that replacing meat with a plant-based alternative may help with weight control.
For tried and tested health and weight loss tips, see the V-Plan Diet (£2.00 plus p&p) and the guide 5:2 Vegan Style (£1.00 plus p&p). Call 0117 944 1000 or visit www.vivashop.org.uk to order.
5. Get Smart – Lose the Flab!
Weight loss might not only help cut dementia risk but also boost brain power, according to a study published in the journal Neurology. Researchers from Toulouse University Hospital in France tested the cognitive ability in over 2,200 healthy workers aged 32 to 62. Middle-aged adults with a high BMI scored less on cognitive tests than those with a low BMI. For example, a test involving word memory recall showed that those with a BMI of 20 (considered healthy) remembered an average of nine out of 16 words, while those with a BMI of 30 (classed as obese) remembered an average of seven out of 16 words. Study author Dr Maxime Cournot suggested that these findings may be due to a host of factors including the thickening and hardening of cerebral vessels because of obesity, or possibly the development of insulin resistance.
6. Juice may Cut Alzheimer’s Risk
Research suggests that drinking fruit and vegetable juices frequently may cut the risk of developing Alzheimer’s disease. In a study published in the American Journal of Medicine, US and Japanese scientists followed almost 2,000 people for up to 10 years. Risk for Alzheimer’s was a massive 76 per cent lower among those who drank juice more than three times a week, compared with those who drank it less than once weekly. They concluded that fruit and vegetable juices may play an important role in delaying the onset of Alzheimer’s disease, particularly among those who are at high risk for the disease.
7. Alzheimer’s Disease… Good Fat
People who eat omega-3 fatty acids may have a lower risk of Alzheimer’s later in life say researchers from Aberdeen University. 120 over-64s were given written intelligence tests and gave blood samples for analysis. There was a clear link between better results and the presence of omega-3s, but only in those missing a particular gene thought to predispose to Alzheimer’s. In those with the gene present, the omega-3 fats made no difference to their test scores.
Omega-3s are a type of polyunsaturated fat. Good vegetarian sources include flaxseeds (linseeds), walnuts and their oils.
8. Alzheimer’s Disease… Bad Fat
People with high cholesterol levels in mid-life are more likely to develop Alzheimer’s than those with low cholesterol, according to new research from California. From a group of 9,752 people (whose cholesterol had been measured in their 40s) 504 developed Alzheimer’s. Those with high cholesterol levels in mid-life were 50 per cent more likely to develop this disease later in life.
9. Calcium in Dairy Linked to Dementia
Too much calcium may lead to dementia in the elderly, new research reveals. Scientists found that excess calcium in the diet can narrow the blood vessels in the brain leading to tissue damage (lesions) that may cause cognitive impairment, dementia, depression and stroke. The brains of 79 men and 153 women aged between 60 and 86 were scanned, and all were found to have a number of lesions. The findings, presented at the Experimental Biology meeting in Washington DC, suggest that the calcium in dairy foods may be responsible.
The same US team previously showed that people who consume high levels of fatty dairy produce have more lesions but fat intake alone was not a factor. This study provides support to the growing number of researchers concerned about the effects of too much calcium, particularly in older adults.
10. Alzheimer’s and the Link with Meat
Symptoms of Alzheimer’s are very similar to the brain-destroying infection Creutzfeltd Jakob disease (vCJD), the human form of mad cow disease. And there’s little difference between them according to a recent book by Dr Murray Waldman, Toronto’s coroner, who claims that Alzheimer’s may well be caused by a rogue protein called a prion in much the same way that vCJD is. More than this, he believes the source of vCJD and Alzheimer’s is identical – meat!
Waldman sets out his reasons. In all prion diseases the brain is affected by dense deposits and dementia is the major symptom. In most cases these symptoms don’t show until later in life and prior to that there are no indications that people are incubating the disease. There is no way of reversing it once it starts. Prion diseases were first described in medical literature around the start of the 20th century. The majority of cases are in the developed world with very few in countries such as India, Bangladesh and Nigeria. All these factors are true for Alzheimer’s also.
Waldman charts the growth of the meat industry and meat eating and relates this directly to the number of cases – the more meat, the more cases of Alzheimer’s. The World Health Organisation’s figures for meat consumption correlate almost exactly with Waldman’s theory.
The organisations which were set up to represent AD victims must surely have made a similar connection? It seems not. “Both diseases involve proteins in the brain that somehow change shape and cause damage,” says Dr Susanne Sorensen, head of research for the Alzheimer’s Society. “But they are different proteins and the diseases have a different biochemistry and a different pathology.”
So what is the cause? “Many of the risk factors for heart disease also apply to Alzheimer’s.”
It still puts meat squarely in the frame as those risk factors are saturated fat, cholesterol, high levels of a substance called homocysteine and high blood pressure, all caused largely by animal products.
Such an immediate rejection of the idea that prions may be involved seems a little arrogant considering that the man who discovered them, and won a Nobel Prize for his efforts, Professor Stanley Prusiner, believes they may well be. If this eminent scientist’s instincts are correct then the way to avoid Alzheimer’s entirely is to stop eating meat. If he’s wrong and Dr Sorensen is right, the way to dramatically reduce your risk is to stop eating not just meat but dairy products also, along with seafood and eggs.
Dr Margaret Rayman (Oxford Project to Investigate Memory and Ageing – Optima) has brought together all this advice into a recommended diet to avoid the devastating disease that is Alzheimer’s. It is, of course, entirely vegan and contains no animal products at all.
Further Resources
To obtain copies of the resources listed in this information sheet, contact Viva!Health: 0117 944 1000; www.viva.org.uk or by post: Viva!Health, 8 York Court, Wilder Street, Bristol BS2 8QH.
References
- Lancet. 369 (9557) 208-16. Davey et al., 2002. EPIC–Oxford: lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meateaters in the UK.
- Public Health Nutrition. 6(3) 259–268. Haddad EH, Berk LS, Kettering JD et al, 1999. Dietary intake and biochemical, hematologic, and immune status of vegans compared to non-vegetarians. Am J Clin Nutr 70(Suppl): 86S-593S
- Whalley, L.J., Deary, I.J., Starr, J.M., Wahle, K.W., Rance, K.A., Bourne, V.J. and Fox, H.C. 2008. n-3 Fatty acid erythrocyte membrane content, APOE varepsilon4, and cognitive variation: an observational follow-up study in late adulthood. American Journal of Clinical Nutrition. 87 (2) 449-454.
- Gale et al., 2007. IQ in childhood and vegetarianism in adulthood: 1970 British cohort study. British Medical Journal. 334 (7587) 245.
- Whitmer RA, Gunderson EP, Barrett-Connor E, Quesenberry CP Jr, Yaffe K. 2005. Obesity in middle age and future risk of dementia: a 27 year longitudinal population based study. The British Medical Journal. 330 (7504) 1360
- Gustafson D, Rothenberg E, Blennow K, Steen B, Skoog I. 2003. An 18-year follow-up of overweight and risk of Alzheimer disease. Archives of Internal Medicine. 163 (13) 1524-8
- Newby PK, Tucker KL, Wolk A. 2005. Risk of overweight and obesity among semivegetarian, lactovegetarian, and vegan women. The American Journal of Clinical Nutrition. 81 (6) 1267-74
- Barnard ND, Scialli AR, Turner-McGrievy G, Lanou AJ, Glass J. 2005. The effects of a low-fat, plant-based dietary intervention on body weight, metabolism, and insulin sensitivity. The American Journal of Medicine. 118 (9) 991-7.
- Presentation: Midlife Serum Total Cholesterol and Risk of Alzheimer s Disease and Vascular Dementia Three Decades Later; Solomon, A., Kuopio, Finland, Kivipelto, M., Stockholm, Sweden, Zhou, J., Whitmer, R.A., Oakland, CA. American Academy of Neurology 60th Anniversary Annual Meeting, Chicago, 16 April 2008.
This post has been categorised in: All Print Materials, Factsheets




