Plant-based Diets and Cardiovascular Disease Factsheet
Have a Heart – Go Vegan!
Cardiovascular disease (CVD) such as heart disease and stroke is the number one killer in the UK and globally. More people are living with it than ever before and numbers are steadily rising. Viva! Health investigates the causes of CVD and explains how a vegan diet can be used to both prevent and treat the UK’s biggest health problem.
What is cardiovascular disease?
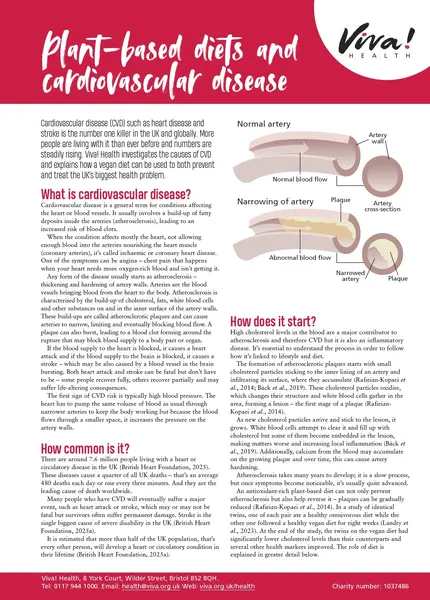
Cardiovascular disease is a general term for conditions affecting the heart or blood vessels. It usually involves a build-up of fatty deposits inside the arteries (atherosclerosis), leading to an increased risk of blood clots.
When the condition affects mostly the heart, not allowing enough blood into the arteries nourishing the heart muscle (coronary arteries), it’s called ischaemic or coronary heart disease. One of the symptoms can be angina – chest pain that happens when your heart needs more oxygen-rich blood and isn’t getting it.
Any form of the disease usually starts as atherosclerosis – thickening and hardening of artery walls. Arteries are the blood vessels bringing blood from the heart to the body. Atherosclerosis is characterised by the build-up of cholesterol, fats, white blood cells and other substances on and in the inner surface of the artery walls. These build-ups are called atherosclerotic plaques and can cause arteries to narrow, limiting and eventually blocking blood flow. A plaque can also burst, leading to a blood clot forming around the rupture that may block blood supply to a body part or organ.
If the blood supply to the heart is blocked, it causes a heart attack and if the blood supply to the brain is blocked, it causes a stroke – which may be also caused by a blood vessel in the brain bursting. Both heart attack and stroke can be fatal but don’t have to be – some people recover fully, others recover partially and may suffer life-altering consequences.
The first sign of CVD risk is typically high blood pressure. The heart has to pump the same volume of blood as usual through narrower arteries to keep the body working but because the blood flows through a smaller space, it increases the pressure on the artery walls.
Insert image from the old factsheet – atherosclerosis (healthy blood vessel and one with plaque)
How common is it?
There are around 7.6 million people living with a heart or circulatory disease in the UK (British Heart Foundation, 2025). These diseases cause a quarter of all UK deaths – that’s an average 480 deaths each day or one every three minutes. And they are the leading cause of death worldwide.
Many people who have CVD will eventually suffer a major event, such as heart attack or stroke, which may or may not be fatal but survivors often suffer permanent damage. Stroke is the single biggest cause of severe disability in the UK (British Heart Foundation, 2025a).
It is estimated that more than half of the UK population, that’s every other person, will develop a heart or circulatory condition in their lifetime (British Heart Foundation, 2025a).
How does it start?
High cholesterol levels in the blood are a major contributor to atherosclerosis and therefore CVD but it is also an inflammatory disease. It’s essential to understand the process in order to follow how it’s linked to lifestyle and diet.
The formation of atherosclerotic plaques starts with small cholesterol particles sticking to the inner lining of an artery and infiltrating its surface, where they accumulate (Rafieian-Kopaei et al., 2014; Bäck et al., 2019). These cholesterol particles oxidise, which changes their structure and white blood cells gather in the area, forming a lesion – the first stage of a plaque (Rafieian-Kopaei et al., 2014).
As new cholesterol particles arrive and stick to the lesion, it grows. White blood cells attempt to clear it and fill up with cholesterol but some of them become embedded in the lesion, making matters worse and increasing local inflammation (Bäck et al., 2019). Additionally, calcium from the blood may accumulate on the growing plaque and over time, this can cause artery hardening.
Atherosclerosis takes many years to develop; it is a slow process, but once symptoms become noticeable, it’s usually quite advanced.
An antioxidant-rich plant-based diet can not only prevent atherosclerosis but also help reverse it – plaques can be gradually reduced (Rafieian-Kopaei et al., 2014). In a study of identical twins, one of each pair ate a healthy omnivorous diet while the other one followed a healthy vegan diet for eight weeks (Landry et al., 2023). At the end of the study, the twins on the vegan diet had significantly lower cholesterol levels than their counterparts and several other health markers improved. The role of diet is explained in greater detail below.
Risk factors
Some people have genes that make them more susceptible to heart disease but lifestyle is what matters most. More often than not, it’s not about the genes that run in the family but about the diet and lifestyle that children inherit from their parents.
The main risk factors for heart disease include:
- High blood pressure – a risk factor but also often the first symptom, tightly linked to diet and lifestyle
- High cholesterol levels – the more cholesterol is in the blood, the more building material is available for plaque formation; the amount of cholesterol in the blood can be significantly influenced by the diet
- Smoking – the harmful substances resulting from tobacco smoking can damage blood vessels and increase plaque formation
- Physical inactivity – the less we move about, the less exercise our circulatory system gets. For blood vessels to stay healthy, it’s important that they are stimulated by different levels of activity
- Being overweight or obese – this factor has a lot to do with diet and physical inactivity
- Diabetes – high blood sugar levels can directly damage blood vessels and increase cholesterol levels
- Alcohol consumption – excessive alcohol intake can increase your cholesterol levels and blood pressure and contribute to weight gain
- Family history – if your male relatives developed heart disease before the age of 55 and/or your female relatives developed it before the age of 65, it is considered a family history of heart disease
- Ethnic background – in the UK, people of south Asian and Black African or African Caribbean background have an increased risk of heart disease compared to the White European population
- Age – the older we get, the higher the risk
- Gender – men generally tend to develop heart disease at a younger age than women
For atherosclerotic plaques to develop, building materials are needed and we either do or don’t supply those through diet. In the following sections, you’ll find why high cholesterol, high blood pressure and excessive body weight are the main risk factors for heart disease and how they are affected by diet.
Cholesterol
Cholesterol is a waxy substance made by the liver. We need some to build cell membranes and produce hormones, vitamin D and bile. The problem starts when there’s too much of it.
Cholesterol travels through the bloodstream bound with proteins and other fat molecules in special transport vehicles called lipoproteins. These are the main two that you may have heard of:
- Low-density lipoprotein (LDL) contains a large cholesterol load and is known as ’bad’ cholesterol because it is strongly associated with the build-up of plaques.
- High-density lipoprotein (HDL) is called ‘good’ cholesterol because it returns cholesterol back to the liver for removal.
Cholesterol returned to the liver is mostly turned into bile acids – a major component of bile – that help us digest fats in the small intestine. Some cholesterol also directly passes into the bile and with it, into the small intestine. Much of the bile acids and some cholesterol is then absorbed again in the small intestine and circulates back into the body, while the rest is excreted in our faeces.
High levels of cholesterol in the blood are a significant risk factor for developing heart and circulatory diseases. When total and LDL cholesterol levels are increased, there’s plenty of building material for plaques to develop and grow. On the other hand, it’s good when HDL cholesterol levels are increased as that means cholesterol is being cleared away.
What your cholesterol levels should be:
- Total cholesterol: below 5 mmol/L or 193 mg/dL
- HDL (good cholesterol): above 1 mmol/L or 39 mg/dL
- Non-HDL (bad cholesterol): below 4 mmol/L or 155 mg/dL – this is total cholesterol minus HDL because all non-HDL cholesterol is considered a risk factor
- LDL (bad cholesterol): below 3 mmol/L or 116 mg/dL
It’s estimated that close to a half of all adults in the UK are living with high cholesterol levels – greater than 5mmol/L (British Heart Foundation, 2024a).
Dietary cholesterol and blood cholesterol
Animals, just like us, make their own cholesterol and it’s a basic component of their cell membranes so all animal products – meat, fish, shellfish, eggs and dairy – contain it. Eggs are the richest dietary source of cholesterol with just one egg containing an average 187 milligrams. Plant foods do not contain any cholesterol whatsoever.
We absorb 20 to 80 per cent of the cholesterol in food, depending on our genes (Stellaard, 2022). However, even in people who have low-cholesterol-absorbing genes, dietary cholesterol can still increase blood levels if consumed together with high amounts of saturated fat (Kang and Zivkovic, 2022). Most animal products, such as meat, fish or high-fat dairy, contain both, while others may be combined in a way that delivers both cholesterol and saturated fats in one meal – for example, eggs with a buttered toast or chicken fried in butter, lard or coconut oil.
Plant compounds similar in structure but not function to cholesterol – sterols and stanols – compete with cholesterol for absorption in the gut and so lower the amount of cholesterol absorbed (Stellaard, 2022). That’s why there are so many products enriched with plant sterols (also called phytosterols) and marketed as ‘cholesterol-lowering’. However, a diet based on plant foods achieves this reduction naturally.
A recent study of different dietary groups from Germany – meat-eaters, flexitarians, vegetarians and vegans – found that while meat-eaters ate around 400 milligrams of cholesterol a day, vegans had only a negligible intake and vegans also had less than half the saturated fat intake compared to meat-eaters (Dawczynski et al., 2022). In this study, vegans had almost 25 per cent lower levels of total cholesterol and 27 per cent lower levels of LDL cholesterol than meat-eaters. Other studies have found similar results (Yokoyama et al., 2017).
Different types of fat
Fats are divided into separate categories based on the structure of the fatty acids they contain. The chemical bonds within each fatty acid can be either saturated or unsaturated and this also determines their activity in the body.
Saturated fats – we don’t need these in our diet as our bodies can make them and high intakes increase blood cholesterol levels. The main sources of saturated fat are animal products (meat, fish, shellfish, eggs, dairy products, butter, lard, pies, pastries, processed foods and high-fat spreads), coconut oil and palm fat. Saturated fats are usually solid at room temperature.
Monounsaturated fats – these are not essential in the diet but not harmful as a part of a balanced diet. Monounsaturated fats are found in many plants and vegetable oils. Probably the most common one is oleic acid – an omega-9 fat – the main component of olive, macadamia, avocado and sunflower oil.
Polyunsaturated fats – these are the essential omega-6 and omega-3 fats – we need them for good health. The main omega-6 fat is linoleic acid found in seeds, nuts, corn, pulses and soya oil. Most people in the UK consume plenty of omega-6 fats and need to increase the intake of omega-3s.
Omega-3 fats from plants come in the form of ALA (alpha-linolenic acid) which our bodies convert to EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). Rich sources of ALA are ground flaxseed, hempseed, chia seeds, walnuts and rapeseed oil. Microalgae and fish oils contain ready-made EPA and DHA – out of the two, algae-derived omega-3 supplements are a much healthier choice because they are not contaminated with dangerous pollutants and are sustainable.
Trans/hydrogenated fats – these fats have a different structure to all other fats and are dangerous to heart health because they raise blood cholesterol levels more than other types of fat. See more information below.
Saturated fats and cholesterol
It’s well-established that a diet high in saturated fats increases blood cholesterol levels – in particular, the dangerous LDL type (Kris-Etherton and Krauss, 2020). While the mechanisms of how this works are still unclear, many studies show higher saturated fat intakes are linked to higher cholesterol levels and when they are replaced by unsaturated fats, cholesterol levels drop.
For example, a large study combining the results from the Nurses’ Health Study and the Health Professionals Follow-Up Study, including data from over 127,000 people (Li et al., 2015) found that replacing just five per cent of energy from saturated fats with polyunsaturated fats, monounsaturated fats or carbohydrates from wholegrains was associated with a 25 per cent, 15 per cent and nine per cent lower risk of coronary heart disease, respectively.
A highly respected Cochrane review on the subject found that cutting down on saturated fat led to a 17 per cent lower risk of cardiovascular events – including heart disease, heart attacks and strokes (Hooper et al., 2020). When the UK-based Scientific Advisory Committee on Nutrition reviewed all available evidence in 2019, they came to the conclusion that reducing saturated fat intake reduces the risk of heart and circulatory disease and lowers cholesterol levels. They suggest that “reducing population average saturated fat intakes from current levels of intake to no more than about 10 per cent of [total] dietary energy would result in health benefits to the population”.
Another comprehensive study was undertaken by the American Heart Association, examining the effect of saturated fats on heart health. Their Presidential Advisory paper states that replacing saturated fats in the diet with polyunsaturated fats achieves a significant reduction in cardiovascular events (Sacks et al., 2017). This dietary change can reduce the risk of heart disease and related events by about 30 per cent, which is a reduction similar to that achieved by the cholesterol-lowering drugs called statins.
How about tropical oils – coconut and palm?
While most plant oils are low in saturated fats, palm and coconut oils are exceptions – they are very rich sources. Coconut oil is made up of more than 80 per cent saturated fats, while the figure for palm oil is 50 per cent (similar to butter) and for palm kernel oil, 80 per cent. Palm oil is made from the palm fruit while palm kernel oil comes from the seeds and both can be used in foods or food preparation, such as frying.
Despite many misleading claims, these so-called tropical oils raise LDL cholesterol levels and the risk of heart disease (Sun et al., 2015; Sacks et al., 2017; Neelakantan et al., 2020). Some studies show that coconut oil doesn’t raise cholesterol levels as much as animal fats but because it raises LDL cholesterol nevertheless, it cannot be recommended as a healthy oil (Eyres et al., 2016; Santos et al., 2019).
When it comes to palm oil, it raises both LDL and HDL cholesterol, which is why some argue that its health effects may not be as detrimental as with saturated fats of animal origin (Unhapipatpong et al., 2021) but major health institutions, such as the American Heart Association, disagree and warn against its consumption (Sacks et al., 2017).
Trans fats, cholesterol and atherosclerosis
Trans fats are naturally found in small amounts in the meat and milk of ruminant animals (cattle, sheep, goats) but can also be man-made when liquid vegetable oils are hydrogenated to make them solid or semi-solid at room temperature. These industrial trans fats are frequently used in processed foods or for frying and are usually listed as hydrogenated fats, partially hydrogenated fats (or fatty acids) or trans fats.
Trans fats raise cholesterol levels even more than saturated fats and are considered a risk factor for heart disease. The reason for their detrimental effect is thought to be that they slow down the natural breakdown of LDL cholesterol and increase the breakdown of HDL cholesterol – this leads to increased total and LDL cholesterol levels, which is a dangerous scenario as it facilitates the build-up of atherosclerotic plaques (Sacks et al., 2017; Oteng and Kersten, 2020). On top of that, trans fat consumption also increases inflammation in blood vessels further contributing to plaque growth (Oteng and Kersten, 2020).
A major review published in the British Medical Journal reported that even a low intake of trans fatty acids was associated with a 21 per cent higher risk of heart disease and a 28 per cent higher risk of dying from heart disease (de Souza et al., 2015).
Note on margarine: margarine used to contain hydrogenated fats but most manufacturers have changed their ingredients and production methods, so margarine is now a healthy butter alternative (always check the ingredients).
Your diet can slash cholesterol levels
Diet plays a major role in how high or low our cholesterol levels are and many studies suggest what we should be eating to lower and maintain healthy cholesterol levels.
The American Society for Preventive Cardiology states that saturated fats increase total and LDL cholesterol and should be avoided (Belardo et al., 2022). However, a heart-healthy diet means much more than just replacing saturated fats.
Plant-based diets based around wholegrains, fruit and vegetables, pulses, nuts and seeds and unsaturated fats have been shown time and again to be effective at lowering and keeping blood cholesterol levels down – vegan diets in particular (Trautwein and McKay, 2020). This effect is thought to be due to the fact that these diets are high in fibre, healthy complex carbohydrates, plant protein, unsaturated fats, antioxidants and plant sterols, while at the same time being low in saturated and trans fats, sugar and cholesterol.
A scientific review of 40 studies revealed that vegans consumed 50 per cent less saturated fat than meat-eaters, had significantly lower LDL cholesterol levels and had lower blood pressure (Benatar and Stewart, 2018). And there are other studies showing similar results (Bradbury et al., 2014; Yokoyama et al., 2017; Landry et al., 2024).
Three scientific studies examining the effect of wholefood vegan diet for 12 to 16 weeks found remarkably similar results (Kahleova et al., 2021; Barnard et al., 2022; Chiu et al., 2022). The participants’ total cholesterol dropped by 1.0 to 1.2 mmol/l (18.7 to 28 mg/dL) and LDL cholesterol by 0.8 to 1.4 mmol/l (15.3-26 mg/dL) – very powerful results.
And a vegan diet brings even better results than the Mediterranean diet, often recommended for heart disease patients. A study comparing a vegan Mediterranean diet to the traditional form of this diet (that includes some animal products) showed that the vegan diet was clearly superior (López-Moreno et al., 2024). It produced greater cholesterol reduction, including lowering LDL cholesterol levels.
When a scientific team investigated the effects of a diet high in red meat, then white meat and then no meat on participants’ cholesterol levels, their results were clear – both red and white meat increased cholesterol levels but a meat-free diet did not (Bergeron et al., 2019). The study also tested the effect of additional saturated fat – they added high-fat dairy products, including butter, to the participants’ diet – and found that it increased cholesterol levels in all groups.
High blood pressure
Blood pressure is always recorded with two numbers – the systolic pressure (higher number) is the force at which your heart pumps blood into the body and the diastolic pressure (lower number) is the resistance to the blood flow in the blood vessels (the force of the blood pushing against the wall of blood vessels). They are both measured in millimetres of mercury (mmHg).
A healthy blood pressure is usually considered to be between 90 and 120 mmHg for the systolic pressure and 60 to 80 mmHg for the diastolic pressure. If your blood pressure is 140/90 mmHg or higher, it is considered to be high blood pressure, also called hypertension. An estimated 30 per cent of UK adults have high blood pressure, which means around 16 million people (British Heart Foundation, 2025a).
High blood pressure is closely linked with high cholesterol levels because cholesterol plaques cause narrowing of the arteries so the heart has to pump harder to push blood through. High blood pressure puts extra strain on blood vessels, heart, brain, kidneys and eyes and increases the risk of blood vessel damage in these organs.
The main risk factors for hypertension include an unhealthy diet, being overweight, high salt intake, excessive alcohol or caffeine consumption, smoking, insomnia and other sleep disturbances, being over 65 years of age, genetics (some people naturally have higher blood pressure) and being of black African or black Caribbean descent. Thankfully, many of these are preventable.
High cholesterol levels can lead to atherosclerosis over time, which then causes high blood pressure, but if you don’t have regular blood tests, you may not know anything is wrong.
In most cases, medication alone may not be sufficient to lower both blood pressure and cholesterol to levels considered healthy, so lifestyle changes, including a diet based on plant foods, are essential to achieve meaningful risk reduction (Borghi et al., 2022).
High blood pressure and diet
As part of a large, long-running study examining the impact of lifestyle and diet on blood pressure – the INTERMAP study – researchers studied people who consistently show low levels of cardiovascular risk factors (Shay et al., 2012). They discovered that these people have certain dietary traits in common – a higher intake of plant protein, fibre, magnesium (plentiful in plant foods), non-haem iron (plant iron), potassium (also plentiful in plant foods), lower overall energy intake, lower intake of cholesterol, saturated fats, animal protein and salt compared with people who are at a higher risk of cardiovascular disease.
Another part of the study focused only on plant-based diets and found that healthy diets (favouring wholegrains, fruits, vegetables, nuts, pulses and vegetable oils) are linked to lower blood pressure, while unhealthy plant-based diets (favouring processed foods, desserts, sweetened beverages and potato products) can increase it (Aljuraiban et al., 2020).
One study compiled and analysed data from three large prominent studies to determine what effect different types of meat have on blood pressure (Borgi et al., 2015). It revealed that one serving of red or processed meat daily increased the risk of hypertension by 30 per cent and one serving of poultry increased it by 22 per cent.
On the other hand, across scientific studies, vegans consistently have lower blood pressure than other diet groups (Alexander et al., 2017; Chiu et al., 2020) and when compared with meat-eaters, vegans have a 63 per cent lower risk of high blood pressure (Pettersen et al., 2012).
In people who suffer from high blood pressure, a switch to a wholefood plant-based diet usually achieves a significant reduction in blood pressure and cholesterol (McDougall et al., 2014; Alexander et al., 2017; Campbell et al., 2019; Joshi et al., 2019; Lee et al., 2020). So convincing is the evidence that a recent review concluded that doctors should recommend a healthy plant-based diet as a means for both prevention and treatment of high blood pressure (Charles et al., 2024).
Another benefit of a wholefood vegan diet is the increased intake of dietary nitrates – natural compounds found in vegetables, particularly in green leafy vegetables and beetroot. They help blood vessels relax and so lower blood pressure. In a study of over 50,000 participants followed for 23 years, those with the highest dietary nitrate intake had markedly lower blood pressure (Bondonno et al., 2021).
Nitrates used as preservatives and to colour bacon, for example, do not have a beneficial effect on heart health. In fact, they can combine with proteins in processed meats to create nitrosamines, which are associated with an increased risk of cancer. Studies show that eating vegetables rich in natural nitrates may reduce your risk of chronic disease, whereas eating foods high in added nitrates can increase health risks.
Obesity and heart disease
The American Heart Association states in their review of the evidence that obesity directly contributes to cardiovascular risk factors, including high cholesterol and triglyceride levels, high blood pressure, blood vessel inflammation, increased blood clotting, impaired blood sugar control and also sleep disorders (Powell-Wiley et al., 2021). They highlight that obesity can lead to the development of cardiovascular disease and potentially fatal events, independently of other cardiovascular risk factors. Obese people tend to develop heart disease and experience serious cardiovascular events at an earlier age and have a shorter life span than people of a healthy weight.
Abdominal obesity – large waist circumference – is considered a particular risk and is linked with fat storage in the liver and around the heart. The longer a person carries this excess fat, the higher the risk of heart disease and related events (Powell-Wiley et al., 2021). Inflammation induced by obesity increases LDL cholesterol oxidation, which leads to faster plaque formation and undermines normal functioning of blood vessels.
An extensive study examining the health of 300,000 people found that being overweight increases your risk of heart disease by 32 per cent, while obesity raises it by 81 per cent (Bogers et al., 2007).
Diet and lifestyle modifications are paramount to tackling obesity and reducing the health risks associated with it. A wholesome vegan diet can be a true life-changer for obese and overweight people because it not only makes us healthier, improves metabolism and achieves gradual weight-loss, it does so without portion restriction (Najjar and Feresin, 2019; Kahleova et al., 2020).
When we look at body weight across different dietary groups, vegans are the only ones with consistently healthy weight and are best protected from obesity (Rizzo et al., 2013; Tantamango-Bartley et al., 2013; Le and Sabaté, 2014; Huang et al., 2016).
Gut bacteria and heart health
The bacteria that live in our gut can have wide-ranging effects on our health, including the risk of heart disease. There are trillions of bacteria and what we eat determines which species thrive and which decline. Healthy gut bacteria help us digest food and keep our gut healthy but there can also be harmful bacteria that produce toxic by-products that can damage the gut wall integrity and cause inflammation.
Beneficial gut bacteria thrive on fibre-rich foods (plant wholefoods) and produce a substance called butyrate and other short-chain fatty acids (SCFAs). These products help maintain healthy function of the gut wall and are anti-inflammatory (Kazemian et al., 2020; Trøseid et al., 2020; Witkowski et al., 2020). Other beneficial bacteria convert cholesterol into a substance called coprostanol, which is excreted with faeces – that way, these bacteria help to lower cholesterol levels (Tomova et al., 2019; Kazemian et al., 2020).
On the other hand, potentially harmful gut bacteria thrive on meat, eggs, high-fat and fried foods, processed foods, sugar and alcohol and produce toxins that can damage the gut wall, cause local inflammation and get into our bloodstream, causing inflammation in the blood vessels, which contributes to atherosclerosis (Kazemian et al., 2020; Trøseid et al., 2020; Malesza et al., 2021). These bacteria and their products can also compromise the integrity of the gut wall, resulting in the substances from the gut leaking into the bloodstream and undermining our health (Witkowski et al., 2020).
Some bacteria produce a substance called trimethylamine (TMA) from foods rich in L-carnitine (meat) and choline (eggs) and the liver then turns that into trimethylamine N-oxide (TMAO) (Campbell, 2017; Spence, 2018; Witkowski et al., 2020). TMAO is dangerous because it increases the stickiness of cholesterol particles, changes cholesterol metabolism in the liver for the worse and also stimulates platelet activity, which may increase blood clot formation (Chiu et al., 2020; Kazemian et al., 2020; Trøseid et al., 2020). Studies show that people with the highest levels of TMAO have a 2.5-fold higher risk of major cardiovascular events (heart attack or stroke) than people with the lowest levels (Tang et al., 2013; Witkowski et al., 2020).
Diet plays a big role in the composition of gut bacteria and their products entering our bloodstream – research reveals that the differences can be truly profound and that meat-eaters produce TMAO at a much higher rate than vegans (Koeth et al., 2019). What’s more, a healthy vegan diet can significantly reduce TMAO in people whose levels are high – by around 50 per cent (Witkowski et al., 2020; Argyridou et al., 2021)).
As all the above studies agree, eating plenty of fibre-rich plant wholefoods is key to a healthy gut bacteria population, which, in turn, is key for the reduction of heart disease risk.
Omega-3 fats, fish oils and heart disease
Omega-3 fats are essential for us – we need them for good health because they are a natural component of many of our tissues. However, how much they also protect us from heart disease is not entirely clear.
Cochrane reviews are considered to be the gold standard quality in science. The most comprehensive Cochrane review of evidence on the subject found that increasing EPA and DHA has little or no effect on cardiovascular events (eg heart attack) or death (Abdelhamid et al., 2020). They also found that omega-3 supplements do not reduce the risk of heart disease, stroke or death caused by cardiovascular events and that there was little evidence of any effects of eating fish. However, eating ALA (from flaxseed or flaxseed oil, chia seeds, hemp seed, walnuts or rapeseed oil) may help slightly reduce cardiovascular events, heart irregularities and death. They concluded that increasing plant‐based ALA may be mildly protective for some heart and circulatory diseases.
An earlier review showed that regular ALA intake lowered the risk of cardiovascular disease developing by about 10 per cent and the risk of fatal events by 20 per cent (Pan et al., 2012). And a recent review revealed that ALA intake is linked to lower cholesterol levels, blood pressure and markers of inflammation (Sala-Vila et al., 2022).
When it comes to fish oil supplements, another scientific review found a concerning effect – they may actually increase the risk of atrial fibrillation (irregular heartbeat) by 25 per cent and if you take more than one gram daily, the risk may increase by 49 per cent (Gencer et al., 2021). On the other hand, ALA from plants reduces the risk (Abdelhamid et al., 2020).
Heart-healthy diet
According to the American Society for Preventive Cardiology, 90 per cent of cardiovascular risk is attributable to nine factors: abnormal blood fats (high cholesterol and triglycerides), smoking, high blood pressure, diabetes, abdominal obesity, psychosocial factors, low consumption of fruit and vegetables, too much alcohol and a lack of regular physical activity (Belardo et al., 2022). They recommend a diet focusing on fruit, vegetables, pulses, nuts, seeds, plant protein and omega-3 fat sources, as well as replacing saturated fat with unsaturated, reducing dietary cholesterol intake and increasing intake of fibre-rich foods. The European Society of Cardiology recommendations are virtually the same and they also highlight that sugar intake should be minimised and trans fats are to be avoided completely (Visseren et al., 2021). The American Heart Association’s guidance also falls in line with both of these (Lichtenstein et al., 2021).
Vegan diets are the perfect answer to this as they are associated with lower cholesterol and triglyceride levels, lower blood pressure, healthy body weight and lower levels of inflammatory markers (Mehta et al., 2023; Landry et al., 2024).
Plants contain a wide range of antioxidants that help protect blood vessels from damage, tone down inflammation, decrease LDL cholesterol oxidation and can improve blood sugar control (Korakas et al., 2018). A wholefood vegan diet is naturally low in saturated fat, devoid of cholesterol, high in fibre and healthy carbohydrates, and contains healthy unsaturated fats, natural nitrates (that help dilate blood vessels), a wealth of antioxidants and other health-protective compounds, and supports the growth of health-beneficial gut bacteria – all of these factors are the reason why it’s so beneficial for the heart (Kahleova et al., 2017; Satija and Hu, 2018; Gan et al., 2021).
In a recent review of plant-based diets and cardiovascular health, the authors concluded that studies consistently show that plant-based diets reduce the risk of heart disease and stroke (Del Re and Aspry, 2022). They highlighted that to achieve this effect, the diet has to be healthy and not based on processed and sugary foods. This is an important distinction because, as a large Harvard University study of almost 200,000 people showed, a healthy plant-based diet can reduce the risk of heart disease by 25 per cent, while an unhealthy one may increase the risk (Satija et al., 2017).
Research is clear – diets high in meat, saturated fats, sugar, junk foods and salt, and lacking in fruit and vegetables, wholegrains, pulses, nuts and seeds can greatly contribute to cardiovascular disease and fatal cardiovascular events. A healthy vegan diet, on the other hand, can protect our cardiovascular system better than any other diet.
Stress and heart disease
Short-term stress, such as being nervous about a meeting or getting scared by a dangerous situation, is normal and harmless for a healthy person because once the situation passes, the stress is gone. However, for people who already have some heart or circulatory issues, even short-term stress can be dangerous (Osborne et al., 2020; Levine, 2022). It’s because stress causes blood vessels to constrict and that increases blood pressure – if an artery is already narrowed by plaques, a further constriction might block it and lead to sudden events, such as heart attack.
Long-term or chronic stress (lasting months or years), on the other hand, can play a major role in the development of heart disease and cause sudden events even in a healthy person and makes matters worse for heart disease patients (Osborne et al., 2020; Levine, 2022). Chronic stress can be caused, for example, by a difficult living or financial situation, bereavement, lasting physical or mental health problems, a stressful job or family issues.
In response to stress, which is perceived as danger by the body, the sympathetic nervous system is activated and the hormones cortisol and adrenaline are released. These cause an increase in blood pressure, blood lipids (including cholesterol) and blood sugar because they are preparing the body for a fight or flight and so it’s important that muscles are well-supplied with oxygen and energy. At the same time, the immune system is blunted while pro-inflammatory substances are released and blood clotting increases (Osborne et al., 2020). When there’s no fight or flight and the stressful situation continues, it may lead to a lasting increase in blood pressure, blood sugar, cholesterol levels and triglycerides, and cause or contribute to inflammation in blood vessels, which promotes the build-up of atherosclerotic plaques (Levine, 2022). At the same time, the increased blood clotting poses a risk, especially in people who already have atherosclerosis, because a blood clot can block an artery.
As a part of a heart-healthy lifestyle, it’s important to engage in stress management techniques, such as non-competitive physical activity, mindfulness, yoga, meditation, calming breathing exercises, etc.
Viva! Health’s Six Steps for a Healthy Heart
1) Eat only plant-based foods, focus on wholefoods
This rule naturally follows from all the official recommendations for a heart-healthy diet. A fully vegan diet is the best for your heart and blood vessels.
In practice, it means building your diet from wholegrain foods (wholemeal bread, oats, wholewheat pasta, brown rice, quinoa, rye crackers), pulses (beans, lentils, soya, chickpeas, peas and products made from them), fruit and vegetables, nuts and seeds. Older studies focused on low-fat diets but newer evidence shows that choosing the right kind of fat is more important than reducing all fat. Avoid adding lots of oil to your meals but there’s no need to avoid nut butters or the occasional avocado. Green leafy vegetables, such as kale, cabbage, rocket, broccoli, watercress or Brussels sprouts, reduce arterial stiffness and blood pressure and have an anti-inflammatory effect (Freeman et al., 2018). Put them on your daily menu.
2) Minimise refined flour, sugar, processed foods, excess salt and alcohol
These foods may be vegan but are not healthy and can even raise your risk of heart disease. Keep their consumption to a minimum or cut them out completely. This means avoiding foods such as white bread, cakes, pastries, sugary or salty processed snacks, anything deep-fried, sugar-sweetened beverages and alcoholic drinks. Processed foods that contain hydrogenated or partially hydrogenated fats should be avoided altogether.
3) Daily dose of omega-3s
It’s important to get your daily dose of the essential omega-3 fats because not only are they needed for healthy cells and tissues but they also support healthy gut bacteria and tone down inflammation in your blood vessels.
A daily dose of ALA (1.1 grams for women and 1.6 grams for men) can be obtained from any one of the following:
- A heaped tablespoon of ground flaxseed OR two teaspoons of flaxseed oil
- A heaped tablespoon of chia seeds – it’s best to let them soak a little or blend them in a smoothie to make their nutrients more available
- Two tablespoons of shelled hempseed
- Ten walnut halves
- Two tablespoons of rapeseed oil (used for cooking or baking)
OR you can take an algae-derived supplement providing 250 to 500 milligrams of EPA and DHA combined.
4) Take the essential supplements
We need a regular supply of vitamins B12 and D for our bodies to work as they should. They are essential for everyone and because they are hard to obtain from diet, many people have low levels or are deficient.
For vitamin B12, take a daily dose providing 50 micrograms or a weekly dose providing 2,000 micrograms. Lack of vitamin B12 can lead to hyperhomocysteinemia – too much homocysteine in the blood. Homocysteine is a metabolic product of the amino acid methionine and it is further processed with the help of vitamins B6, B12 and folate. A lack of vitamin B12 can lead to high levels of homocysteine in the blood which can damage the lining of the arteries and may also make the blood clot more easily, which can increase the risk of blood vessel blockages and contribute to cholesterol plaque build-up, increasing the risk of heart disease and stroke (Chiu et al., 2020).
Vitamin D is either obtained from the diet or made in the skin following exposure to sunlight. However, having fortified foods such as plant milks, cereals and margarines may not be enough for everyone and some people may need a supplement from October to April because our skin simply cannot make enough. During warmer months, your skin can probably make sufficient vitamin D when exposed to natural sunlight, unless you spend your days indoors or always cover your skin, in which case you may need a supplement all year long. The recommended daily dose is 10 micrograms or 400 IU (international units).
5) Be active
Physical activity is a simple yet very effective heart-protector. It can be in the form of a daily 30-minute walk, a moderate workout twice or three times a week, any outdoor activity that increases your heart rate, or indoor exercise, yoga, Pilates or even housework if you do it vigorously!
6) Practice stress management
Stress can be bad news for your heart and circulation. We cannot avoid stress but we can use smart tools to help us deal with it – for example, breathing exercises, mindfulness techniques, meditation, arts, music or gardening.
Even if your diet is perfect, you don’t smoke or drink alcohol, keep your salt intake low and engage in physical activity, you can still be at high risk of cardiovascular events if your stress levels are high and unregulated.
A vegan diet can save your life
A number of scientific reviews found that vegan and vegetarian diets lower your risk of heart disease by 18 to 41 per cent (Appleby and Key, 2016; Dinu et al., 2017; Kahleova et al., 2017; Glenn et al., 2019; Dybvik et al., 2023; Ocagli et al., 2023) – with vegan diets typically bringing better results. If you also add some exercise, don’t smoke, avoid excessive drinking and practice stress management, your risk will be even lower. A vegan diet won’t make you bulletproof but it can certainly do wonders for your heart.
References
Abdelhamid AS, Brown TJ, Brainard JS et al. 2020. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Systematic Reviews. 3(3):CD003177.
Alexander S, Ostfeld RJ, Allen K, Williams KA. 2017. A plant-based diet and hypertension. Journal of Geriatric Cardiology. 14 (5) 327-330.
Aljuraiban G, Chan Q, Gibson R et al. – INTERMAP Research Group. 2020. Association between plant-based diets and blood pressure in the INTERMAP study. BMJ Nutrition, Prevention and Health. 3 (2) 133-142.
Appleby PN, Key TJ. 2016. The long-term health of vegetarians and vegans. Proceedings of the Nutrition Society. 75 (3) 287-293.
Argyridou S, Davies MJ, Biddle GJH et al. 2021. Evaluation of an 8-week vegan diet on plasma trimethylamine-N-oxide and post-challenge glucose in adults with dysglycaemia or obesity. Journal of Nutrition. 151 (7) 1844-1853.
Bäck M, Yurdagul A Jr, Tabas I et al. 2019. Inflammation and its resolution in atherosclerosis: mediators and therapeutic opportunities. Nature Reviews. Cardiology. 16 (7) 389-406.
Barnard ND, Alwarith J, Rembert E et al. 2022. A Mediterranean diet and low-fat vegan diet to improve body weight and cardiometabolic risk factors: A randomized, cross-over trial. Journal of the American Nutrition Association. 41 (2) 127-139.
Belardo D, Michos ED, Blankstein R et al. 2022. Practical, evidence-based approaches to nutritional modifications to reduce atherosclerotic cardiovascular disease: An American Society For Preventive Cardiology clinical practice statement. American Journal of Preventive Cardiology. 10, 100323.
Benatar JR, Stewart RAH. 2018. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS One. 13 (12) e0209086.
Bergeron N, Chiu S, Williams PT et al. 2019. Effects of red meat, white meat, and nonmeat protein sources on atherogenic lipoprotein measures in the context of low compared with high saturated fat intake: a randomized controlled trial. American Journal of Clinical Nutrition. 110 (1) 24-33.
Bogers RP, Bemelmans WJ, Hoogenveen RT et al. – BMI-CHD Collaboration Investigators. 2007. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Archives of Internal Medicine. 167 (16) 1720-1728.
Bondonno CP, Dalgaard F, Blekkenhorst LC et al. 2021. Vegetable nitrate intake, blood pressure and incident cardiovascular disease: Danish Diet, Cancer, and Health Study. European Journal of Epidemiology. 36 (8) 813-825.
Borghi C, Fogacci F, Agnoletti D, Cicero AFG. 2022. Hypertension and dyslipidemia combined therapeutic approaches. High Blood Pressure and Cardiovascular Prevention. 29 (3) 221-230.
British Heart Foundation. 2025. Facts and figures. [online]. Available from: bhf.org.uk/what-we-do/news-from-the-bhf/contact-the-press-office/facts-and-figures
British Heart Foundation. 2025a. BHF Statistics Factsheet – UK.
Campbell T. 2017. A plant-based diet and stroke. Journal of Geriatric Cardiology. 14 (5) 321-326.
Campbell EK, Fidahusain M, Campbell Ii TM. 2019. Evaluation of an eight-week whole-food plant-based lifestyle modification program. Nutrients. 11 (9) 2068.
Charles JA, Habibullah NK, Bautista S et al. 2024. Planting the seed for blood pressure control: The role of plant-based nutrition in the management of hypertension. Current Cardiology Reports. 26 (3) 121-134.
Chiu THT, Chang HR, Wang LY, et al. 2020. Vegetarian diet and incidence of total, ischemic, and hemorrhagic stroke in 2 cohorts in Taiwan. Neurology. 94(11) e1112-e1121.
Chiu THT, Kao YC, Wang LY et al. 2022. A dietitian-led vegan program may Improve GlycA, and other novel and traditional cardiometabolic risk factors in patients with dyslipidemia: A pilot study. Frontiers in Nutrition. 9, 807810.
de Souza RJ, Mente A, Maroleanu A et al. 2015. Intake of saturated and trans unsaturated fatty acids and risk of all-cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 351, h3978.
Del Re A, Aspry K. 2022. Update on plant-based diets and cardiometabolic risk. Current Atherosclerosis Reports. 24 (3) 173-183.
Dinu M, Abbate R, Gensini GF et al. 2017. Vegetarian, vegan diets and multiple health outcomes: A systematic review with meta-analysis of observational studies. Critical Reviews in Food Science and Nutrition. 57 (17) 3640-3649.
Dybvik JS, Svendsen M, Aune D. 2023. Vegetarian and vegan diets and the risk of cardiovascular disease, ischemic heart disease and stroke: a systematic review and meta-analysis of prospective cohort studies. European Journal of Nutrition. 62 (1) 51-69.
Eyres L, Eyres MF, Chisholm A, Brown RC. 2016. Coconut oil consumption and cardiovascular risk factors in humans. Nutrition Reviews. 74 (4) 267-80.
Freeman AM, Morris PB, Aspry K et al. 2018. A clinician’s guide for trending cardiovascular nutrition controversies: Part II. Journal of the American College of Cardiology. 72 (5) 553-568.
Gencer B, Djousse L, Al-Ramady OT et al. 2021. Effect of Long-Term Marine ɷ-3 Fatty acids supplementation on the risk of atrial fibrillation in randomized controlled trials of cardiovascular outcomes: A systematic review and meta-analysis. Circulation. 144 (25) 1981-1990.
Glenn AJ, Viguiliouk E, Seider M et al. 2019. Relation of vegetarian dietary patterns with major cardiovascular outcomes: a systematic review and meta-analysis of prospective cohort studies. Frontiers in Nutrition. 6, 80.
Hooper L, Martin N, Jimoh OF et al. 2020. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database of Systematic Reviews. 8 (8) CD011737.
Huang J, Liao LM, Weinstein SJ et al. 2020. Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Internal Medicine. 180 (9) 1173-1184.
Joshi S, Ettinger L, Liebman SE. 2019. Plant-based diets and hypertension. American Journal of Lifestyle Medicine. 14 (4) 397-405.
Kahleova H, Levin S, Barnard N. 2017. Cardio-metabolic benefits of plant-based diets. Nutrients. 9 (8) 848.
Kahleova H, Petersen KF, Shulman GI et al. 2020. Effect of a low-fat vegan diet on body weight, insulin sensitivity, postprandial metabolism, and intramyocellular and hepatocellular lipid levels in overweight adults: A randomized clinical trial. JAMA Network Open. 3 (11) e2025454.
Kang JW, Zivkovic AM. 2022. Are eggs good again? A precision nutrition perspective on the effects of eggs on cardiovascular risk, taking into account plasma lipid profiles and TMAO. Journal of Nutritional Biochemistry. 100, 108906.
Kazemian N, Mahmoudi M, Halperin F et al. 2020. Gut microbiota and cardiovascular disease: opportunities and challenges. Microbiome. 8 (1) 36.
Koeth RA, Lam-Galvez BR, Kirsop J et al. 2019. l-Carnitine in omnivorous diets induces an atherogenic gut microbial pathway in humans. Journal of Clinical Investigations. 129 (1) 373-387.
Korakas E, Dimitriadis G, Raptis A, Lambadiari V. 2018. Dietary composition and cardiovascular risk: A mediator or a bystander? Nutrients. 10 (12) 1912.
Kris-Etherton PM, Krauss RM. 2020. Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES. American Journal of Clinical Nutrition. 112 (1) 13-18.
Landry MJ, Ward CP, Cunanan KM et al. 2023. Cardiometabolic effects of omnivorous vs vegan diets in identical twins: A randomized clinical trial. JAMA Network Open. 6 (11) e2344457.
Landry MJ, Senkus KE, Mangels AR et al. 2024. Vegetarian dietary patterns and cardiovascular risk factors and disease prevention: An umbrella review of systematic reviews. American Journal of Preventative Cardiology. 20, 100868.
Le LT, Sabaté J. 2014. Beyond meatless, the health effects of vegan diets: findings from the Adventist cohorts. Nutrients. 6 (6) 2131-2147.
Lee KW, Loh HC, Ching SM, Devaraj NK, Hoo FK. 2020. Effects of vegetarian diets on blood pressure lowering: A systematic review with meta-analysis and trial sequential analysis. Nutrients. 12 (6) 1604.
Levine GN. 2022. Psychological stress and heart disease: Fact or folklore? American Journal of Medicine. 135 (6) 688-696.
Li Y, Hruby A, Bernstein AM et al. 2015. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: A prospective cohort study. Journal of the American College of Cardiology. 66 (14) 1538-1548.
Lichtenstein AH, Appel LJ, Vadiveloo M et al. 2021. 2021 Dietary guidance to improve cardiovascular health: A scientific statement from the American Heart Association. Circulation. 144 (23) e472-e487.
López-Moreno M, Fresán U, Del Coso J et al. 2024. The OMNIVEG STUDY: Health outcomes of shifting from a traditional to a vegan Mediterranean diet in healthy men. A controlled crossover trial. Nutrition, Metabolism and Cardiovascular Diseases. 34 (12): 2680-2689.
Malesza IJ, Malesza M, Walkowiak J et al. 2021. High-fat, Western-style diet, systemic inflammation, and gut microbiota: A narrative review. Cells. 10 (11) 3164.
McDougall J, Thomas LE, McDougall C et al. 2014. Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort. Nutrition Journal. 13, 99.
Mehta P, Tawfeeq S, Padte S et al. 2023. Plant-based diet and its effect on coronary artery disease: A narrative review. World Journal of Clinical Cases. 11 (20) 4752-4762.
Najjar RS, Feresin RG. 2019. Plant-based diets in the reduction of body fat: Physiological effects and biochemical insights. Nutrients. 11 (11) 2712.
Neelakantan N, Seah JYH, van Dam RM. 2020. The effect of coconut oil consumption on cardiovascular risk factors: A systematic review and meta-analysis of clinical trials. Circulation. 141 (10) 803-814.
Ocagli H, Berti G, Rango D et al. 2023. Association of vegetarian and vegan diets with cardiovascular health: an umbrella review of meta-analysis of observational studies and randomized trials. Nutrients. 15 (19) 4103.
Osborne MT, Shin LM, Mehta NN et al. 2020. Disentangling the links between psychosocial stress and cardiovascular disease. Circulation. Cardiovascular Imaging. 13 (8) e010931.
Oteng AB, Kersten S. 2020. Mechanisms of Action of trans Fatty Acids. Advances in Nutrition. 11 (3) 697-708.
Pan A, Chen M, Chowdhury R et al. 2012. α-Linolenic acid and risk of cardiovascular disease: a systematic review and meta-analysis. American Journal of Clinical Nutrition. 96 (6) 1262-73.
Pettersen BJ, Anousheh R, Fan J et al. 2012. Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Public Health Nutrition. 15 (10) 1909-1916.
Powell-Wiley TM, Poirier P, Burke LE et al. – American Heart Association Council on lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. 2021. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation. 143 (21) e984-e1010.
Rafieian-Kopaei M, Setorki M, Doudi M et al. 2014. Atherosclerosis: process, indicators, risk factors and new hopes. International Journal of Preventative Medicine. 5 (8) 927-46.
Rizzo NS, Jaceldo-Siegl K, Sabate J, Fraser GE. 2013. Nutrient profiles of vegetarian and non-vegetarian dietary patterns. Journal of the Academy of Nutrition and Dietetics. 113 (12) 1610-1619.
Sacks FM, Lichtenstein AH, Wu JHY et al. – American Heart Association. 2017. Dietary fats and cardiovascular disease: A presidential advisory from the American Heart Association. Circulation. 136 (3) e1-e23.
Sala-Vila A, Fleming J, Kris-Etherton P et al. 2022. Impact of α-linolenic acid, the vegetable ω-3 fatty acid, on cardiovascular disease and cognition. Advances in Nutrition. 13 (5) 1584-1602.
Santos HO, Howell S, Earnest CP, Teixeira FJ. 2019. Coconut oil intake and its effects on the cardiometabolic profile – A structured literature review. Progress in Cardiovascular Disease. 62 (5) 436-443.
Satija A, Bhupathiraju SN, Spiegelman D et al. 2017. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. Journal of the American College of Cardiology. 70 (4) 411-422.
Scientific Advisory Committee on Nutrition (SACN). 2019. Saturated fats and health. Available from: gov.uk/government/publications/saturated-fats-and-health-sacn-report
Shay CM, Stamler J, Dyer AR et al. 2012. Nutrient and food intakes of middle-aged adults at low risk of cardiovascular disease: the international study of macro-/micronutrients and blood pressure (INTERMAP). European Journal of Nutrition. 51 (8) 917-926.
Spence JD. 2018. Diet for stroke prevention. Stroke and Vascular Neurology. 3 (2) 44-50.
Stellaard F. 2022. From dietary cholesterol to blood cholesterol, physiological lipid fluxes, and cholesterol homeostasis. Nutrients. 14 (8) 1643.
Sun Y, Neelakantan N, Wu Y et al. 2015. Palm Oil Consumption Increases LDL Cholesterol Compared with Vegetable Oils Low in Saturated Fat in a Meta-Analysis of Clinical Trials. Journal of Nutrition. 145 (7) 1549-1558.
Tang WH, Wang Z, Levison BS et al. 2013. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. New England Journal of Medicine. 368 (17) 1575-1584.
Tantamango-Bartley Y, Jaceldo-Siegl K, Fan J, Fraser G. 2013. Vegetarian diets and the incidence of cancer in a low-risk population. 2013. Cancer Epidemiology, Biomarkers & Prevention. 22 (2) 286-294.
Tomova A, Bukovsky I, Rembert E et al. 2019. The effects of vegetarian and vegan diets on gut microbiota. Frontiers in Nutrition. 6, 47.
Trautwein EA, McKay S. 2020. The role of specific components of a plant-based diet in management of dyslipidemia and the impact on cardiovascular risk. Nutrients. 12 (9) 2671.
Trøseid M, Andersen GØ, Broch K, Hov JR. 2020. The gut microbiome in coronary artery disease and heart failure: Current knowledge and future directions. EBioMedicine. 52, 102649.
Unhapipatpong C, Shantavasinkul PC, Kasemsup V et al. 2021. Tropical oil consumption and cardiovascular disease: An umbrella review of systematic reviews and meta analyses. Nutrients. 13 (5) 1549.
Visseren FLJ, Mach F, Smulders YM et al. – ESC National Cardiac Societies; ESC Scientific Document Group. 2021. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal. 42 (34) 3227-3337.
Witkowski M, Weeks TL, Hazen SL. 2020. Gut microbiota and cardiovascular disease. Circulation Research. 127 (4) 553-570.
Yokoyama Y, Levin SM, Barnard ND. 2017. Association between plant-based diets and plasma lipids: a systematic review and meta-analysis. Nutrition Reviews. 75 (9) 683-698.
This post has been categorised in: All Print Materials, Factsheets




