Talking Thyroid Facts
Why iodine is important and vegetarian/vegan food support a healthy thyroid
This factsheet is available online only.
The thyroid helps control how quickly we use up the energy we get from food. What happens when is doesn’t work properly? How important is iodine? What other nutrients do we need for a healthy thyroid? Can soya foods disrupt the thyroid? We answer all these questions and more.
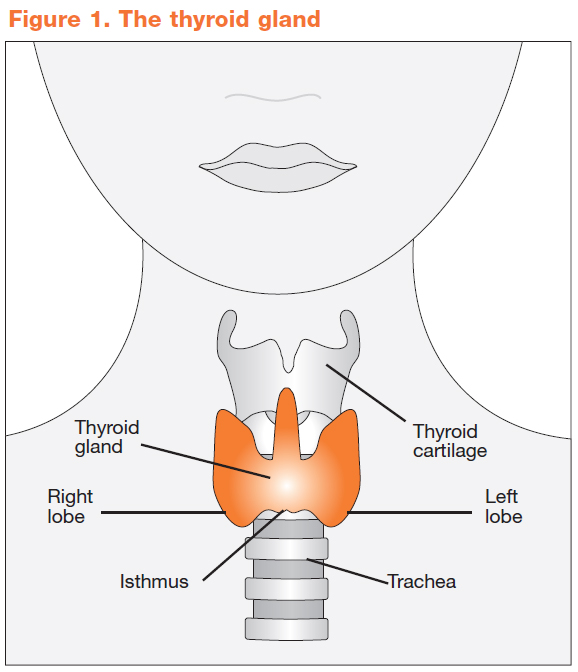
The thyroid gland
The thyroid (Fig. 1) is a small endocrine gland found in the front of the neck. It produces the hormones thyroxine (T4) and triiodothyronine (T3) and calcitonin and secretes them into the bloodstream. Thyroxine and triiodothyronine are extremely important for the regulation of the body’s metabolism, affecting heart rate, body temperature and help control how fast the body uses energy from food. Calcitonin helps control the level of calcium in the blood. Every cell in the body depends upon thyroid hormones for regulation of their metabolism.
Thyroid hormones
Around 80 to 90 per cent of the hormone released from the thyroid gland is thyroxine. The thyroid also produces triiodothyronine, which has about four times the hormone ‘strength’ as thyroxine. But most triiodothyronine is generated in the body by removing a single iodine atom from thyroxine. This happens naturally in the body as required. The thyroid gland is controlled by the pituitary gland, which is the size of a peanut and is located at the base of the brain. When the level of thyroid hormones (T3 and T4) dip too low, the pituitary gland produces thyroid stimulating hormone (TSH) which stimulates the thyroid gland to produce more hormones, so raising their blood levels. The pituitary senses this and responds by decreasing its TSH.
An overactive or underactive thyroid (the most common problems of the thyroid) can disrupt the levels of hormone produced and lead to serious health problems.
Overactive thyroid
Hyperthyroidism (also known as thyrotoxicosis or overactive thyroid), is a condition that occurs when there are too many thyroid hormones in the body. This causes the body to use up energy from food faster; as a result metabolism is accelerated. The condition is more common in women than men (NHS Choices, 2010).
Symptoms of hyperthyroidism
- Difficulty breathing
- Hyperactivity
- Mood swings, irritability and nervousness
- Difficulty sleeping
- Fatigue (extreme tiredness)
- Muscle weakness
- Needing to pass stools (faeces) or urine frequently
- Diarrhoea or streatorrhoea (excess fat in your stools)
- Sensitivity to heat and excess sweating
- Increased appetite
- Sudden weight loss or gain
- Very infrequent, or light periods, or periods stopping altogether
- Infertility
- Loss of interest in sex
Source: NHS Choices, 2010a.
If you have diabetes, you may also find that your diabetic symptoms, such as extreme thirst and tiredness, are made worse by hyperthyroidism.
Signs of hyperthyroidism
If you have hyperthyroidism, you may notice some of the following physical signs:
- A swelling in your neck caused by an enlarged thyroid gland (goitre)
- Uncoordinated rhythm between your heartbeat and pulse
- A rapid resting heart rate
- A tremor (trembling or shaking)
- Warm, moist skin
- Redness on the palms of your hands
- Loosening of your nails in their nail beds
- Itchy skin with raised itchy swellings (urticaria)
- Patchy hair loss (diffuse alopecia)
- Twitching in your face and limbs
Source: NHS Choices, 2010a.
Some symptoms, such as excessive sweating and the inability to tolerate a hot environment are directly due to heat generated within the body by increased metabolic activity. Weight loss reflects use of body stores of nutrients, as normal food intake cannot keep up with demand (ehealthMD, 2009). Symptoms vary from person to person. For reasons not understood, older individuals with hyperthyroidism often have far fewer symptoms compared to younger people.
Causes of hyperthyroidism
The most common cause of hyperthyroidism is Graves’ disease; an autoimmune inflammatory disorder in which the body’s immune system targets the thyroid causing it to produce excess hormone. It can run in families and can occur at any age, although it is most common in women between 20-40 years of age (NHS Choices, 2010b). In some people who have heart disease, untreated hyperthyroidism places additional stress on the heart, causing problems such as heart failure, irregular heartbeat (atrial fibrillation), or abnormal heart rhythm (arrythmia). Uncontrolled it may also cause osteoporosis (brittle bones). If untreated, it can be fatal. However, drug therapy, radiotherapy and on occasion, surgery have all been used effectively to control an overactive thyroid. A useful description of each option is available from: www.nhs.uk/Conditions/Thyroid-overactive/Pages/Treatment.aspx
Underactive thyroid
Hypothyroidism (or an underactive thyroid), is when not enough thyroid hormones are produced. When the condition occurs from birth it is called congenital hypothyroidism. The adult form of this condition (also known as myxoedema) affects 15 in every 1,000 women and one in every 1,000 men (NHS Choices, 2010c).
Symptoms of hypothyroidism
- General tiredness
- Excessive need of sleep
- Increased awareness of the cold
- The skin may become dry and thick and feels cold
- The hair may begin to thin out and become dry and coarse
- Unusual loss of body hair – eyebrows may become sparse and hair on forearms short and stubbly
- Flaking, splitting nails
- The voice may become hoarse or croaky
- Elevated cholesterol levels
- Constipation
- Muscle weakness, cramps and aches; difficulty climbing stairs
- Sore muscles
- Pins and needles in the fingers and hands
- In women of reproductive years the periods may become heavier and longer, but sometimes can prematurely stop
- Fertility problems – failure to conceive, miscarriage
- Unexplained weight gain
- Puffy face and bags under the eyes, change in facial appearance
- Slow speech, movements and thoughts
- Low mood, depression
- Memory problems and lack of concentration
- Slow heart beat and slightly raised blood pressure
- Anaemia
- Hearing problems
- Swelling at the front of the neck
- Sensation of a lump in the throat
- Although rare, in severe cases, unsteadiness on your feet, mental disturbance and even hallucinations may be experienced
- Loss of libido/impotency
Source: British Thyroid Foundation, 2009.
Children and adolescents
Children with hypothyroidism may have restricted growth. The elderly may develop problems and/or depression. Adolescents may experience precocious puberty, which means going through puberty at an abnormally young age (NHS Choices, 2010d).
Causes of hypothyroidism
Iodine deficiency is the most common cause of hypothyroidism worldwide. However, among people who get sufficient iodine in the diet, the most common cause is an autoimmune reaction, which means your body’s immune system makes antibodies that attack the cells of the thyroid gland, causing inflammation (swelling). This inflammation, or thyroiditis, can result in a damaged thyroid gland that is not able to make enough thyroxine. Hashimoto’s thyroiditis is an example of autoimmune hypothyroidism. It is associated with goitre (a swollen thyroid gland) and runs in families. The second most common cause is the over-treatment of an overactive thyroid with radioactive iodine or surgery (NHS Choices, 2010e).
Thyroid hormones are also suppressed by other factors including:
- Excess oestrogen (or too much oestrogen in relation to progesterone)
- Acute anxiety
- Fatty acid deficiency
- Oxidative stress – free radical damage
- Chronic stress
- Food allergies (eg coeliacs are more likely to develop thyroid problems)
- Toxins, including nicotine and nitrate
- Poor nutrition
Medication (eg lithium and the heart drug amiodarone) Hypothyroidism is normally treated with thyroxine. The vast majority of doctors prescribe the synthetic drug known as levothyroxine for thyroid hormone replacement, which usually results in normal levels of circulating thyroid hormones in the majority of patients. However, many people can take a long time to heal and GPs may not explain the wide range of symptoms caused by this disease. For example, anaemias are diagnosed in 20-60 per cent of patients with hypothyroidism and after diet, thyroid disease is the most common secondary cause of high cholesterol. Depression is also very common in hypothyroid patients.
There is an interesting web site listing ‘top doctors’ for treating thyroid conditions – as recommended by patients (not Viva!Health) at: www.thyroid-info.com/topdrs/unitedkingdom.htm
It can also be helpful consulting a nutritional therapist.
Osteoporosis
Excess thyroid hormone can increase the process of natural bone turnover, whereby bone is continuously broken down and replaced. If this process happens too rapidly, bone-building cells cannot keep up and the rate of bone loss may increase leading to osteoporosis. This may happen in cases of overactive thyroid, where too much hormone is released, or in cases of underactive thyroid, where too much thyroxine is given. This is why it is important to get the level of medication checked regularly.
Iodine deficiency
Iodine is a trace element found in seawater, rocks and some types of soil (FSA, 2009). It is essential for the production of thyroxine (which contains four iodine atoms). So, low levels of iodine can result in low levels of thyroxine. This can cause the pituitary gland (at the base of the skull) to produce more thyroid-stimulating hormone (TSH) in an effort to boost thyroxine production. This makes the thyroid gland work harder to produce more hormone, causing it to enlarge, becoming what is called a goitre. If the lack of iodine is very severe, hypothyroidism can result.
In the UK, this is virtually unheard of as even very poor diets tend to contain enough iodine. In the few cases of iodine-deficiency related goitre reported, supplementation with iodine (kelp) has been shown to bring about shrinkage of goitres (Park et al., 2005).
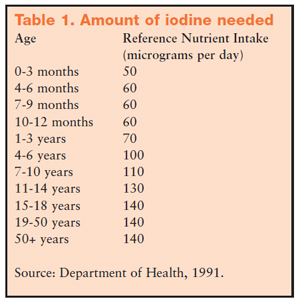
In pregnancy, iodine deficiency can increase the risk of miscarriage, stillbirth and congenital abnormality. People living in areas affected by severe iodine deficiency may have an IQ of up to 13.5 points below that of people from similar communities in areas where there is no iodine deficiency. In its most extreme form, this can result in a condition of severely stunted physical and mental growth (previously called cretinism). On a worldwide basis, iodine deficiency is the single most important preventable cause of brain damage (WHO, 2007). However, of much greater public health importance are the more subtle degrees of brain damage and reduced cognitive ability which can affect populations with a low iodine intake. This is why several different strategies have been employed to eradicate iodine deficiency. To protect against deficiency, the UK Department of Health recommends a Reference Nutrient Intake (RNI) for adults of 140 micrograms of iodine per day (Department of Health, 1991). The RNI is defined as the amount of a nutrient that is sufficient for 97.5 per cent of people in a group. They suggest lower amounts for children (see Table 1).
In 2003 the UK National Diet and Nutrition Survey of adults aged 19 to 64 years found that the average intake of iodine from food sources in men was 215 micrograms and 159 micrograms in women, both over the RNI of 140 micrograms (FSA, 2003). However, they also found that two per cent of men and four per cent of women had an iodine intake that fell below the lower RNI of 70 micrograms per day; the amount of a nutrient that is enough for only a small number of people with low requirements (2.5 per cent). So a small percentage of people clearly need to increase their iodine intake.
Too much iodine
Excess iodine can disrupt thyroid function leading to weight gain, hypothyroidism (with or without goitre), hyperthyroidism and changes in the incidence and types of thyroid cancer (EVM, 2003). This can occur where there is a general high iodine intake or where too much iodine has been given to combat deficiency. It may be argued that the risks of iodine excess are outweighed by the substantial dangers of iodine deficiency. A sensible approach is to supplement the diet at safe levels. The Food Standards Agency (FSA) suggests that 500 micrograms or less a day of iodine supplements is unlikely to cause any harm (FSA, 2009).
Sources of iodine
The major animal food sources of iodine include dairy products and fish. The iodine in cow’s milk and dairy products is not a natural component of these foods, it comes from iodinated cattle feed supplements, iodophor medication, iodine-containing sterilisers of milking equipment, teat dips and udder washes (European Commission Scientific Committee on Food, 2002). Iodine is commonly used as a disinfectant for cleaning surfaces and storage containers. In other words, the dairy cow’s udders are washed with iodine which is why some of it ends up in their milk. As stated, iodine can be found in sea fish and shellfish, although these sources are often contaminated with polychlorinated biphenyls (PCBs), dioxins and mercury. Raw and undercooked fish and shellfish can also contain harmful viruses and bacteria.
Healthier, plant-based sources of iodine include cereals and grains, such as whole wheat and rye. However, levels can vary widely depending on the amount of iodine in the soil where the plants are grown. In general, inland areas and mountainous regions tend to have iodine-poor soil. Iodine may also be present in some green vegetables such as green beans, courgettes, curly kale, spring greens and watercress. However, reliable information on the amount present is difficult to determine due to the variation in soil levels.
Sea vegetables
Long before the discovery of iodine, the beneficial effect of iodine-rich sea vegetables (seaweed) in treating goitre was recognised, first in China and later in medieval Europe. They provide an excellent, healthy source of iodine and many other nutrients including protein, calcium, vitamin A and some B vitamins. Sea vegetables also contain lignans, compounds reported to protect against cancer (Adlercreutz, 2007).
The Okinawan people inhabit a Japanese island in the western Pacific Ocean and are reported to have the longest life expectancy in the world. Their longevity is largely attributed to their plant-based diet in which sea vegetables are eaten every day (Sho et al., 2001). The iodine content of sea vegetables varies very widely. One study analysed 12 different species of sea vegetables and found the iodine content ranged from 16 micrograms per gram in nori to over 8,000 micrograms per gram in one particular sample of processed kelp granules used as a salt substitute (Teas et al., 2004). The authors of this study warned that some sea vegetable dishes may contain excessively high levels of iodine that could disrupt thyroid function.
Given this concern, it is advisable to use small amounts of sea vegetables with a consistent iodine content, such as kelp (kombu). A small amount, often is key. Other sea vegetables such as nori (used in sushi), wakame and arame are relatively low in iodine and can be eaten in moderation without concern about excess iodine. Refer to the packaging for exact figures and recommendations.
In summary, the regular use of small amounts of powdered or crumbled sea vegetables added to soups, stews, salads, pasta dishes or used as a condiment, is an excellent way to ensure a sufficient iodine intake. Alternatively, adults can supplement their diet with kelp tablets but these are not suitable for children. Vecon vegetable stock can contribute to your intake of iodine. However, as 100 grams of Vecon stock contains approximately just 500 micrograms of iodine (Jardox, 2009), you would have to consume 28 grams a day of Vecon to meet your RNI. This is not advisable because of the salt content.
Fighting deficiency
Different strategies have been employed to combat iodine deficiency. In many countries, iodine is added to table salt. In the United States, most table salt contains iodine and Switzerland’s iodised salt programme has been operating uninterrupted since 1922 (Zimmermann, 2008). The iodisation of salt is viewed by many as an enormous success story. Some 91 million newborn infants worldwide are thought to be protected yearly from a significant loss in learning ability as a result of the increased use of iodised salt (UNICEF, 2008). It is currently estimated that 70 per cent of households throughout the world now use iodised salt (WHO, 2007).
However, it could be argued in some countries (with high levels of cardiovascular disease) that linking iodine to salt consumption is questionable. This is because a high salt intake is linked to high blood pressure, which in turn increases the risk of cardiovascular disease (heart attack and stroke). The UK government recommends that adults should eat no more than six grams of salt a day. If you are concerned about your salt intake, you can use kelp as an iodine-rich seasoning instead. Refer to the packaging for guidance on how much to use.
In the UK and other European countries, iodine is added to animal feed. The supplementation of animal feed with iodine is controlled by legislation in the UK with a maximum permitted level of 10 milligrams per kilogram for dairy cattle (MAFF, 2000). Although this maximum limit for iodine was reduced from 40 milligrams per kilogram in July 1996, it is thought that it can cause high intakes of iodine during winter when cattle are fed increased amounts of supplemented foods. A 1998-1999 survey of iodine concentrations in cow’s milk indicated that young children consuming above average amounts of milk could exceed the guideline exposure from milk alone, especially during the winter months (MAFF, 2000). Again, a safer way of ensuring a healthy intake of iodine would be to use a plant-based source such as kelp.
Vegetarian and vegan diets
Iodine deficiency is rare in the UK. However, vegetarian or vegan diets have been blamed by some for the very few cases seen (Remer et al., 1999; Park et al., 2005; Gordon et al., 2006). There has been just one published case of transient neonatal hypothyroidism (where a newborn baby has abnormal thyroid hormone levels at birth, which eventually stabilize and become normal) due to iodine deficiency in the womb. In this case the condition was readily corrected by iodine supplements in the mother and the infant’s condition was corrected by giving thyroxine for just two weeks (Shaikh et al., 2003).
In 1999, a German study suggested that vegetarians who don’t take iodised salt or supplements and eat fruit and vegetables grown in soils with low iodine levels may have a low iodine intake (Remer et al., 1999). Further studies state that vegans may be an ‘at risk’ group for iodine deficiency (Lightowler and Davies, 1998; Krajcovicová-Kudlácková et al., 2003). However, one of these studies also reported that vegans who regularly consume seaweed had intakes in excess of the RNI (but not exceeding the provisional maximum tolerable daily intake level set by the World Health Organisation and the Food and Agricultural Organisation). It may be that as nutritional awareness has increased over the last decade or so, vegetarians and vegans are more likely to ensure a good consistent source of iodine is present in the diet. This may offer advantages over the inconsistent levels provided by diets rich in dairy foods.
Goitrogens
Soya and thyroid function
There are some concerns that soya may interfere with thyroid function. These concerns focus on two substances, goitrogens and isoflavones. Goitrogens occur naturally in many plant foods. They can interfere with the uptake of iodine and lead to a goitre. However, this is not a problem if the diet provides enough iodine. Although a limited number of studies have suggested that soya isoflavones can affect thyroid function, most studies show that soya does not cause problems in people who are healthy and getting enough iodine in their diet. One study showed that supplementing the diet with soya protein (containing soya isoflavones) made no difference to thyroid function in subjects receiving 475 micrograms of iodine per day (Teas et al., 2007).
Furthermore, a review of 14 trials concluded that neither soya protein nor isoflavones adversely affect thyroid function in people with normal thyroid function and sufficient iodine intake (Messina and Redmond, 2006). However, this review did caution that soya foods may interfere with the absorption of synthetic thyroid hormone and so increase the dose of medication required by hypothyroid patients. Furthermore, they warned that infants with congenital hypothyroidism who consume soya infant formula may require higher doses of thyroid medication. One way of mitigating this effect is to separate the time of medication use from feeding as much as possible (easier to achieve in adults than infants). That said, the authors conclude that hypothyroid patients need not avoid soya foods.
In addition, there is a theoretical concern that in individuals with compromised thyroid function or whose iodine intake is low, soya foods may increase the risk of developing hypothyroidism. The general consensus is that all people should ensure their intake of iodine is adequate.
Other Goitrogens
Most goitrogens can stay in the diet, even with hypothyroidism.
- Isothiocyanates. These compounds are primarily found in cruciferous vegetables, such as cabbage, Brussels sprouts, broccoli, cauliflower, mustard greens, kale, turnips and collards. Isothiocyanates, like soya isoflavones, appear to block the enzyme responsible for adding iodine during the production of thyroid hormones, and they may also disrupt signalling across the thyroid’s cell membranes. But no one would argue that these vegetables are bad for you, given that they are filled with vitamins, minerals, antioxidants and avariety of nutrients we all need (aside from being delicious!). These should not be avoided, instead, enjoy them steamed or cooked, as the heat alters the isothiocyanates’ molecular structure and eliminates the goitrogenic effect.
- Gluten is a serious potential goitrogen. Gluten sensitivity has been linked with autoimmune disorders including autoimmune thyroid disease. People with autoimmune-caused hypothyroidism (particularly if they are not responding to their thyroxine medication) may test for gluten allergy (via their GP).
Also:
- Refined foods should be avoided (white bread, pasta, white rice, fizzy drinks, sugary drinks, coffee, jams, crisps, cakes etc).
- Avoid caffeine which stimulates the release of adrenaline, which can negatively affect the thyroid.
Foods to Boost
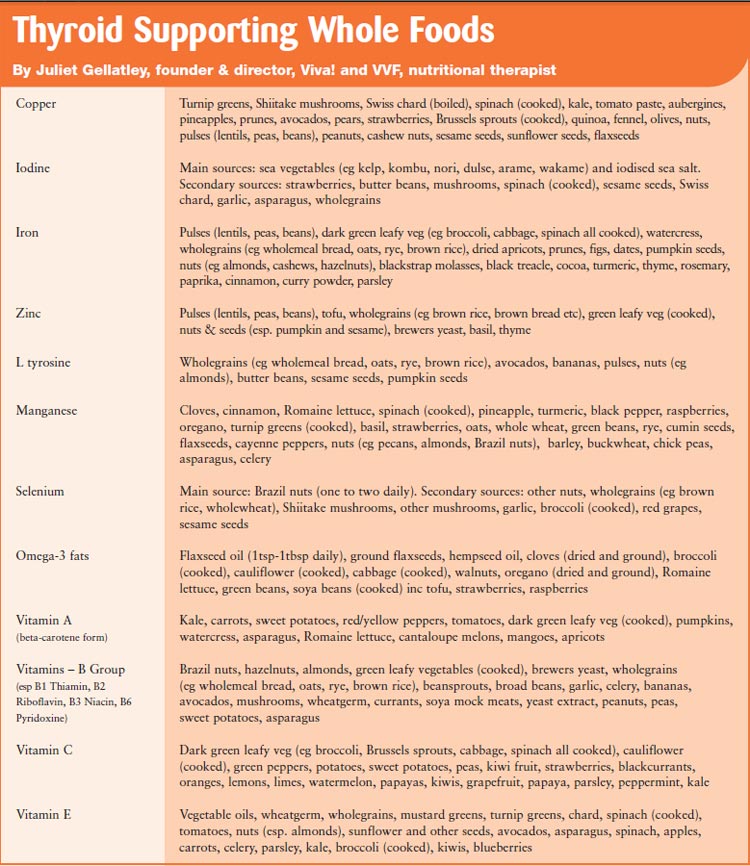
Selenium
Selenium is essential for healthy thyroid function. It is needed for enzymes which help control thyroid hormone synthesis and metabolism; convert thyroxine (T4) into the more accessible form of thyroid hormone, triiodothyronine (T3) and maintain the correct amount of thyroid hormones in the blood and tissues, including the liver, kidneys, and thyroid gland, as well as the brain. Selenium-containing enzymes also function in a protective “detox” capacity, preserving thyroid gland integrity when we’re under stress of all kinds. Selenium also works to help the body more efficiently recycle its iodine stores, which can become an important concern as we grow older.
Zinc, copper and iron
Both hypothyroidism and hyperthyroidism can result in zinc deficiency. When zinc is low in the body, thyroid-stimulating hormone (TSH), T4, and T3 can, in turn, become low in the body. In some cases supplementing with zinc can reverse hypothyroidism.
Copper is needed to produce TSH and T4, so when copper is low in the diet, the rate of T4 production will fail. T4 keeps the body’s cholesterol synthesis on track and it may be that copper deficiency makes people with hypothyroidism more prone to developing high cholesterol and heart problems. As stated iron deficiency anaemia is common in hypothyroidism and so iron-rich foods must be eaten.
Antioxidants and B vitamins
These nutrients are essential for overall good health. Betacarotene (a form of vitamin A), vitamin C and vitamin E, along with selenium and iodine, are important antioxidants that help the thyroid gland neutralise the oxidative stress it encounters on a daily basis. The B vitamins (B2, B3, and B6) are also important for thyroid function because they are involved in manufacturing T4.
Tyrosine
Tyrosine is an amino acid (a building block of protein) required by the body to help manufacture thyroid hormones from iodine.
Summary
- The thyroid is a small gland found in the front of the neck that produces thyroid hormones.
- Thyroid hormones regulate heart rate, body temperature and help control how fast we use food energy.
- An overactive or underactive thyroid can lead to serious health problems.
- Hyperthyroidism (overactive thyroid) can cause hyperactivity, increased appetite, weight loss or gain, irregular heart beat and osteoporosis.
- Hypothyroidism (underactive thyroid) can lead to lethargy, muscle weakness, cramps, a hoarse voice, dry skin, brittle hair, weight gain, periods stopping, anaemia and constipation. More extreme symptoms include deafness, angina and heart failure.
- Hypothyroidism is treated with thyroxine.
- Excess thyroid hormone can lead to osteoporosis which is why it is important to get medication levels checked regularly.
- Iodine (from seawater, rocks and some types of soil and taken up by plants) is essential for the production of thyroxine.
- The UK government suggests that adults need 140 micrograms of iodine per day. Too much can be harmful but up to 500 micrograms a day is unlikely to harm.
- Low iodine intake makes the thyroid gland work harder and can lead to goitre or hypothyroidism.
- In pregnancy, iodine deficiency can increase the risk of miscarriage, stillbirth or congenital abnormality.
- Iodine deficiency is the most common cause of hypothyroidism worldwide and the single most preventable cause of brain damage.
- Too much iodine can disrupt thyroid function leading to weight gain, hypothyroidism, goitre, hyperthyroidism and thyroid cancer.
- Iodine in dairy foods comes from teat dips, udder washes and animal feed; this can result in high levels of iodine intake in big dairy milk consumers.
- Fish and shellfish contain iodine but are often contaminated with PCBs, dioxins and mercury and may also contain viruses and bacteria.
- Many countries use iodised table salt to combat deficiency; this may be a problem for people who need to limit their salt intake.
- Healthier, plant-based sources of iodine include sea vegetables (esp. kale), wholegrains, green vegetables and strawberries, although levels vary widely depending on the amount of iodine in the soil.
- Sea vegetables provide an excellent source of iodine, protein, calcium, beta carotene and some B vitamins. Use sea vegetables with a consistent iodine content, such as kelp (kombu), refer to the packaging for levels and recommendations.
- Adults can supplement their diet with kelp tablets (not suitable for children).
- Vegetarian or vegan diets have been blamed for the very few cases of iodine deficiency seen in the UK. Most vegetarians and vegans get enough iodine in the diet, especially if they include sea vegetables in the diet.
- The concerns that soya may disrupt thyroid are largely unfounded, especially in people with normal thyroid function with sufficient iodine intake.
- Cruciferous vegetables, such as cabbage, Brussels sprouts, broccoli, cauliflower, mustard greens, kale, turnips and collards should be avoided raw in hypothyroidism but their goitrogenic (thyroid disrupting) effect is prevented by cooking.
- Foods to boost to support the thyroid (apart from iodine, see above) include those rich in selenium, zinc, copper, iron, manganese, omega-3 fats, beta-carotene vitamins C, E and B2, B3 and B6, as well the amino acid tyrosine.
References
Adlercreutz, H., 2007. Lignans and human health. 2007. Critical Reviews in Clinical Laboratory Science. 44 (5-6) 483-525.
British Thyroid Foundation, 2009. Signs and Symptoms of Hypothyroidism. Available from: http://www.btf-thyroid.org/ [Accessed 17 November 2009].
Department of Health, 1991. Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report of the Panel on Dietary Reference Values of the Committee on Medical Aspects of Food Policy. London: HMSO.
ehealthMD, 2009. Hyperthyroidism. Available from: http://www.ehealthmd.com/library/hyperthyroidism/HYE_symptoms.html (Accessed 16 November 2009).
European Commission Scientific Committee on Food, 2002. Opinion of the Scientific Committee on Food on the Tolerable Upper Intake Level of Iodine [online]. Available from: www.ceecis.org/iodine/07_legislation/EU%20and%20legislation/eu_upper_iodine_intake.pdf [Accessed 1 April 2009].
EVM, 2003. Expert Group on Vitamins and Minerals. Iodine [online]. Available from: www.food.gov.uk/multimedia/pdfs/evm_iodine.pdf [Accessed 1 April 2009].
FSA, 2009. Iodine [online]. Available from: www.eatwell.gov.uk/healthydiet/nutritionessentials/vitaminsandminerals/iodine/?lang=en [Accessed 1 April 2009].
FSA, 2003. The National Diet & Nutrition Survey: adults aged 19 to 64 years. Volume 3. Vitamin and mineral intake and urinary analytes [online]. Available from: www.food.gov.uk/multimedia/pdfs/ndnsv3.pdf [Accessed 1 April 2009].
Gordon, M., Hall, C. and Rakesh, A., 2006. A rare cause of thyroid goitre in a UK adolescent. Acta Pædiatrica. 95: 1016-1020.
Jardox, 2009. Case, A. (AbbyCase@jardox.com), 10 March 2009. Iodine in Vecon. e-mail to J. Butler (justine@vegetarian.org.uk).
Krajcovicová-Kudlácková, M., Bucková, K., Klimes, I. and Seboková, E. 2003. Iodine deficiency in vegetarians and vegans. Annals of Nutrition and Metabolism. 47 (5) 183-185.
Lightowler, H.J. and Davies, G.J., 1998. Iodine intake and iodine deficiency in vegans as assessed by the duplicate-portion technique and urinary iodine excretion. British Journal of Nutrition. 80 (6) 529-535.
MAFF, 2000. MAFF UK – Iodine In Milk (Sheet 198) [online]. Available from: http://www.ceecis.org/iodine/09_utilisation/02_Animals/09_util_anim_cowsmilk.doc [Accessed 2 June 2009].
Messina, M. and Redmond, G. 2006. Effects of soy protein and soybean isoflavones on thyroid function in healthy adults and hypothyroid patients: a review of the relevant literature. Thyroid. 16 (3) 249-258.
NHS Choices, 2010. Thyroid, overactive [online]. Available from: www.nhs.uk/conditions/Thyroid-overactive/Pages/Introduction.aspx?url=Pages/Whatis-it.aspx [Accessed 12 January 2010].
NHS Choices, 2010a. Symptoms of over-active thyroid. Available from: http://www.nhs.uk/Conditions/Thyroid-over-active/Pages/Symptoms.aspx [Accessed 12 January 2010].
NHS Choices, 2010b. Causes of over-active thyroid. Available from: http://www.nhs.uk/Conditions/Thyroid-over-active/Pages/Causes.aspx [Accessed 12 January 2010].
NHS Choices, 2010c. Thyroid, underactive [online]. Available from: www.nhs.uk/conditions/Thyroid-under-active/Pages/Introduction.aspx?url=Pages/Whatis-it.aspx [Accessed 12 January 2010].
NHS Choices, 2010d. Symptoms of underactive thyroid. Available from: http://www.nhs.uk/Conditions/Thyroid-under-active/Pages/Symptoms.aspx [Accessed 12 January 2010].
NHS Choices, 2010e. Thyroid, underactive, causes [online]. Available from: www.nhs.uk/Conditions/Thyroid-under-active/Pages/Causes.aspx?url=Pages/What-is-it.aspx [Accessed 12 January 2010].
Park, C., Watson, W., Bevan, J. and Abraham, P., 2005. Iodine deficiency goitre in the United Kingdom – the result of a vegan diet. Endocrine Abstracts. 9, 176.
Remer, T., Neubert, A. and Manz, F. 1999. Increased risk of iodine deficiency with vegetarian nutrition. British Journal of Nutrition. 81 (1) 45-49.
Shaikh, M.G., Anderson, J.M., Hall, S.K. and Jackson, M.A., 2003. Transient neonatal hypothyroidism due to a maternal vegan diet. Journal of Pediatric Endocrinology and Metabolism. 16 (1) 111-113.
Sho, H., 2001. History and characteristics of Okinawan longevity food. Journal of Clinical Nutrition. 10, 159.
Teas, J., Pino, S., Critchley, A. and Bravermanm L.E. 2004. Variability of iodine content in common commercially available edible seaweeds. Thyroid. 14 (10) 836-841.
Teas, J., Braverman, L.E., Kurzer, M.S., Pino, S., Hurley, T.G. and Hebert, J.R. 2007. Seaweed and soy: companion foods in Asian cuisine and their effects on thyroid function in American women. Journal of Medicinal Food. 10 (1) 90-100.
UNICEF, 2008. Micronutrients – Iodine, Iron and Vitamin A [online]. Available from: http://www.unicef.org/nutrition/index_iodine.html [Accessed 2 June 2009].
WHO, 2007. World health organisation. Assessment of iodine deficiency disorders and monitoring their elimination [online]. Available from: http://whqlibdoc.who.int/publications/2007/9789241595827_eng.pdf [Accessed 2 April 2009].
Zimmermann, M.B. 2008. Research on iodine deficiency and goiter in the 19th and early 20th centuries. Journal of Nutrition. 138 (11) 2060-2063.
This post has been categorised in: All Print Materials, Factsheets




