Mini factsheet: Crohn’s and colitis
Crohn’s and colitis are inflammatory bowel diseases, Crohn’s can affect anywhere in the gut, colitis occurs in the large bowel.
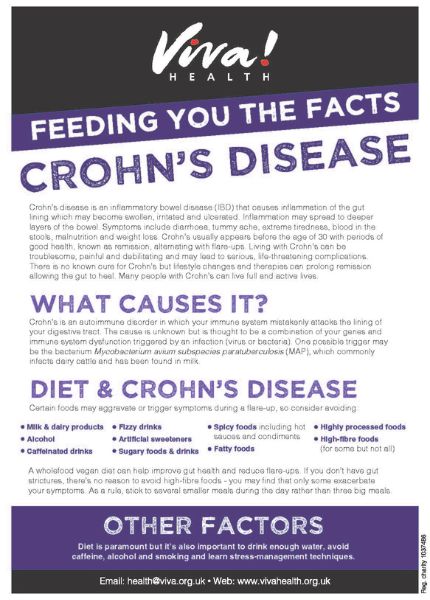
Crohn’s disease
Crohn’s disease is an inflammatory bowel disease (IBD) that causes inflammation of the gut lining which may become swollen, irritated and ulcerated. Inflammation may spread to deeper layers of the bowel.
Symptoms include diarrhoea, tummy ache, extreme tiredness, blood in the stools, malnutrition and weight loss.
Crohn’s usually appears before the age of 30 with periods of good health, known as remission, alternating with flare-ups. Living with Crohn’s can be troublesome, painful and debilitating and may lead to serious, life-threatening complications.
There is no known cure for Crohn’s but lifestyle changes and therapies can prolong remission allowing the gut to heal. Many people with Crohn’s can live full and active lives.
What causes it?
Crohn’s is an autoimmune disorder in which your immune system mistakenly attacks the lining of your digestive tract. The cause is unknown but is thought to be a combination of your genes and immune system dysfunction triggered by an infection (virus or bacteria).
One possible trigger may be the bacterium Mycobacterium avium subspecies paratuberculosis (MAP), which commonly infects dairy cattle and has been found in milk.
Diet and Crohn’s disease
Certain foods may aggravate or trigger symptoms during a flare-up, so consider avoiding:
- Milk and dairy products
- Alcohol
- Caffeinated drinks
- Fizzy drinks
- Artificial sweeteners
- Sugary foods and drinks
- Spicy foods, hot chili sauces and condiments
- Fatty foods
- Highly processed foods
- High-fibre foods (for some but not all)
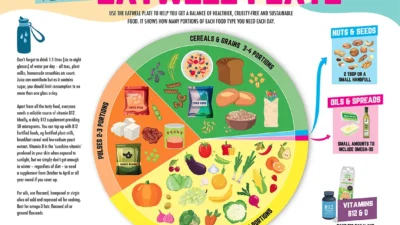
A wholefood vegan diet can help improve gut health and reduce flare-ups. If you don’t have gut strictures, there’s no reason to avoid high-fibre foods – you may find that only some exacerbate your symptoms. As a general rule, stick to several smaller meals during the day rather than three big meals.
Other factors
Diet is paramount but it’s also important to drink enough water, avoid caffeine, alcohol and smoking and learn stress-management techniques.
Colitis
Colitis is inflammation of your colon. Symptoms include tummy ache, bloated stomach, urgent diarrhoea, mucus or blood in your stools, tiredness, loss of appetite and weight loss.
Different types of colitis
There are different types of colitis, depending on what causes it. Some are temporary, such as those caused by a bacterial, viral or parasitic infection and are treatable. However, chronic colitis is a type of inflammatory bowel disease (IBD) and is more difficult to treat.
Ulcerative colitis
Ulcerative colitis is the main type of IBD. Inflammation affects the inner lining of your colon and rectum, creating open sores called ulcers. Symptoms usually come in waves with flare-ups alternating with longer periods of remission. The cause is unknown but is thought to be a combination of genes and immune system dysfunction.
Certain foods and stress can trigger flare-ups but it’s highly individual, so try to track your triggers – common culprits are dairy products and some high-fibre foods, however that’s not a reason to avoid all plant-based wholefoods.
Colitis and diet
Refined carbohydrates, such as white flour and sugar, increase inflammation and should be avoided, but during a flare-up you may tolerate them better than wholefoods. Wholegrains are encouraged but you may find that not all of them agree with you.
Vegetables are mostly well-tolerated but tend to be easier to digest when cooked. They are important for your beneficial gut bacteria that help to tone down inflammation.
On the other hand, protein from meat, cheese, milk, fish and eggs may negatively affect gut bacteria. Choose plant-based protein sources, such as tofu, lentils, beans, nut butters and wholegrains.
There are various diets aimed at helping but no one size fits all, so find what’s right for you, if possible with the guidance of a dietitian or nutritionist experienced with colitis and plant-based diets.
Good to know
Zinc levels are often low in people with IBD so have yours checked and, if needed, normalise them as that may help improve symptoms.
This post has been categorised in: All Print Materials, Mini factsheets